Best Paramedical Training Contains Best Paramedical Course:
HRTD is the best paramedical training center because we conduct the best paramedical course. Paramedical 4-Yeas is the best Paramedical Course among all paramedical training in Bangladesh. Total Course Fee Tk 182500/- including admission fee, semester fee, monthly fee, and exam fee. Total subjects 30 in 4-Years Paramedical Course. 1st Semester contains 5 subjects, 2nd semester contains 5 subjects, 3 semester contains 4 subjects, and 4th semester contains 4 subjects. Each of the rest 4 semesters contains 3 subjects. Total Exam marks 3000.

Best Paramedical Training Course contains huge numbers of practical works:
4-Years Best Paramedial Training Course contains huge practicals like Cardiac Auscultation, Pulmonary Auscultation, Abdominal Auscultation, Cleaning, Dressing, Bandaging, Stitching, Blood Pressure, Hypertension, Hypotension, Systolic Blood Pressure, Diastolic Blood Pressure, Pulse Pressure, Mean Blood Pressure, Heart Beat, Heart Rate, Tachycardia, Bradycardia, Pulse Rate, Radial Pulse, Carotid Pulse, Pulse Oximeter, Oxygen Inhalation, Inhaler, Rotahaler, Nubulizer, Ambo Bag, Oxygen Inhalation from Syllinder, IM Injection, IV Injection, ID Injection, SC Injection, Saline Infusion, Cyanosis Test, Edema Test, Pneumonia Test, Anemia Test, Jaundice Test, Blood Grouping, Blood Collection, Bleeding Time, Clotting Time, Diabetes Test, Percussion, Palpation, etc,
Why 4-Year Paramedical Training Course the Best Paramedical Course?
Actually, Training Curriculums of other Short Paramedical Courses are designed by deducting some subjects and topics from the curriculum of 4-Year Paramedical Training Course. Examples Paramedical 3-Years contains 24 Subjects which is a shorter curriculum than 4-Years Paramedical. Other examples are Paramedical 2-Years and Paramedial 1-Year. Both these Courses contain a short Training Curriculum.

What is a paramedical?
Para means sub and medical means about treatment. So, Paramedical means sub-treatment or more clearly primary treatment. Paramedical courses are designed to provide students with the knowledge and skills necessary to work in the healthcare field. These courses can be taken at various levels, from certificate programs to bachelor’s and master’s degrees, and can lead to a wide range of careers in the medical field.
One of the best paramedical courses available is the Bachelor of Science in Nursing (BSN) program. This program is designed for students who wish to become registered nurses (RNs) and provides them with the knowledge and skills necessary to provide care for patients in a variety of healthcare settings. The BSN program includes both classroom instruction and clinical experience, which allows students to apply the knowledge they have learned in a real-world setting.
Which is the best course in paramedical?
Paramedical courses are designed to provide students with the knowledge and skills necessary to work in the healthcare field. These courses can be taken at various levels, from certificate programs to bachelor’s and master’s degrees, and can lead to a wide range of careers in the medical field.
One of the best paramedical courses available is the Bachelor of Science in Nursing (BSN) program. This program is designed for students who wish to become registered nurses (RNs) and provides them with the knowledge and skills necessary to provide care for patients in a variety of healthcare settings. The BSN program includes both classroom instruction and clinical experience, which allows students to apply the knowledge they have learned in a real-world setting.
Another excellent paramedical course is the Physiotherapy program. Physiotherapy is a healthcare profession that helps people recover from injury, illness, or disability. Physiotherapists work in hospitals, clinics, and community healthcare centers, and help patients to regain movement and function. The program includes both classroom instruction and clinical experience which gives students the hands-on experience they need to become effective practitioners.
Hostel Facilities in HRTD Medical Institute for Best Paramedical Training Center In Bangladesh
Hostal & Meal Facilities
The Institute has hostel facilities for the students. Students can take a bed in the hostel.
Hostel Fee Tk 3000/- Per Month
Meal Charges Tk 3000/- Per Month. ( Approximately )
হোস্টাল ও খাবার সুবিধা
ইনস্টিটিউটে শিক্ষার্থীদের জন্য হোস্টেল সুবিধা রয়েছে। ছাত্ররা হোস্টেলে বিছানা নিতে পারে।
হোস্টেল ফি 3000/- টাকা প্রতি মাসে,
খাবারের চার্জ 3000/- টাকা প্রতি মাসে।(প্রায়)
Address of HRTD Medical Institute for Best Paramedical Training Center In Bangladesh
আমাদের ঠিকানাঃ HRTD মেডিকেল ইন্সটিটিউট, আব্দুল আলী মাদবর ম্যানশন, সেকশন ৬, ব্লোক খ, রোড ১, প্লট ১১, মেট্রোরেল পিলার নাম্বার ২৪৯, ফলপট্টি মসজিদ গলি, মিরপুর ১০ গোলচত্ত্বর, ঢাকা ১২১৬ । মোবাইল ফোন নাম্বার ০১৭৯৭৫২২১৩৬, ০১৯৮৭০৭৩৯৬৫ ।
Our Address: HRTD Medical Institute, Abdul Ali Madbor Mansion, Section-6, Block- Kha, Road- 1, Plot- 11, Metro Rail Pilar No. 249, Falpatty Mosjid Goli, Mirpur-10 Golchattar, Dhaka 1216. Mobile Phone No. 01797522136, 01987073965.
Some Subject for Best Paramedical Training Center In Bangladesh
Paramedical Course subjects. Mobile No. 01987073965, 01797522136.
- Human Anatomy & Physiology-1
- Pharmacology-1
- Study of OTC Drugs
- First Aid-1 & 2
- Practice of Medicine
- Hematology
- Pathology for Medical Practice
- General Surgery-1
- Cardiovascular Anatomy
- Antimicrobial drugs
- Medical Diagnosis-1 & 2
- Chemistry
- Medical Biochemistry
- Orthopedic Anatomy
- Neuro Anatomy & Physiology
Practical Classes And Internship for Best Paramedical Training Center In Bangladesh
Heartbeat, Heart Rate, Cardiac Auscultation, Process of Cardiac Auscultation, Tachycardia, Bradycardia, Pulse, Pulse Rate, Strong Pulse, Weak Pulse, Blood Pressure, Normal Blood Pressure, Systolic Blood Pressure, Diastolic Blood Pressure, Pulse Pressure, Mean Blood Pressure, Hypertension, Hypotension, Hypertension Emergency, First Aid and Management of Hypertension Emergency, Cleaning, Dressing, Bandaging, Stitching, Inhaler, Rotahaler, Nebulizer, Pulse Oxymter, Oxygen Cyllinder, Injection Pushing, IM Injection Pushing, IV Injection Pushing, SC Injection Pushing, Vaccine Pushing, Insulin Pushing, Blood Glucose Masurement, Diabetes, Saline Pushing, Respiratory Meter, First Aid and Management of Shock, First Aid of Bone Fracture, X Ray Report Understanding, Respiration, Respiratory Auscultation, Process of Respiratory Auscultation, First Aid of Diarrhea and Constipation, Dehydration Test, Edema Test, Joundice Test, Anemia Test, etc.
Teachers For Best Paramedical Training Center In Bangladesh
- Dr. Md. Sakulur Rahman, MBBS, CCD (BIRDEM), Course Director
- Dr. Sanjana Binte Ahmed, BDS, MPH, Assistant Course Director
- Dr. Tisha, MBBS, PGT Gyne, Assistant Course Director
- Dr. Suhana, MBBS, PGT Medicine
- Dr. Danial Hoque, MBBS, C-Card
- Dr. Tisha, MBBS
- Dr. Afrin Jahan, MBBS, PGT Medicine
- Dr. Ananna, MBBS
- Dr. Lamia Afroze, MBBS
- Dr. Amena Afroze Anu, MBBS, PGT Gyne, Assistant Course Director
- Dr. Farhana Antara, MBBS,
- Dr. Nazmun Nahar Juthi, BDS, PGT
- Dr. Farhana Sharna, MBBS
- Dr. Bushra, MBBS
- Dr. Turzo, MBBS
- Dr. Kamrunnahar Keya, BDS, PGT (Dhaka Dental College)
- Dr. Shamima, MBBS, PGT Gyne
- Dr. Alamin, MBBS
- Dr. Benzir Belal, MBBS
- Dr. Disha, MBBS
- Dr. Mahinul Islam, MBBS
- Dr. Tisha, MBBS, PGT Medicine
- Dr. Anika, MBBS, PGT
- Dr. Jannatul Ferdous, MBBS, PGT Gyne
- Dr. Jannatul Aman, MBBS, PGT
- Dr. Rayhan, BPT
- Dr. Abu Hurayra, BPT
- Dr. Sharmin Ankhi, MBBS, PGT Medicine
- Md. Monir Hossain, B Pharm, M Pharm
- Md. Monirul Islam, B Pharm, M Pharm
- Md. Feroj Ahmed, BSc Pathology, PDT Medicine
Human Anatomy & Physiology For Best Paramedical Training Center In Bangladesh
The Study of the body Structure and its function is Anatomy & Physiology. Here we discuss the systems of the human body and its organ, Tissues, and cells. The systems of the human body are the digestive system, Respiratory system, Cardiovascular system, Skeletal system, Muscular system, nervous system, Endocrine system, Immune System, Integumentary System and Urinary System.
Human Anatomy and Physiology is the study of the body’s structures (anatomy) and their functions (physiology). Anatomy focuses on the physical arrangement of cells, tissues, organs, and systems, while physiology explains how these structures work together to maintain life processes like movement, metabolism, and reproduction. The two are intertwined, as a structure’s form determines its function, and understanding one requires understanding the other.
Anatomy
- Definition:The scientific study of the body’s structures and their physical arrangement.
- Levels of Study:Can be studied at different levels, including:
- Gross Anatomy: The study of structures visible without a microscope, such as organs and organ systems.
- Microscopic Anatomy (Histology): The study of tissues and cells using a microscope.
- Methods of Study:Historically involved dissection, but now also uses advanced imaging techniques like MRI and CT scans to visualize structures in living people.
Physiology
- Definition: The study of how the body’s structures function to sustain life.
- Key Concepts:
- Complementarity of Structure and Function: The shape and form of a body structure are directly related to what it can do.
- Homeostasis: The body’s ability to maintain a stable internal environment, which is essential for survival.
- Examples: Studying how the heart regulates blood flow or how muscles contract and bring bones together.
Major Body Systems
Understanding human anatomy and physiology involves studying the body’s major systems, including:
Musculoskeletal System, Circulatory System, Nervous System, Digestive System, Respiratory System, Integumentary System, Endocrine System, Lymphatic System, Urinary System, and Reproductive System.
Why It’s Important
- Health Professions:It is a fundamental science for careers in medicine and other health fields.
- Personal Health:Knowledge of the human body helps in making informed health decisions and understanding medical information.
Pharmacology for Best Paramedical Training Center In Bangladesh
The study of drugs and medicines is called Pharmacology, In 1 Year Nursing Course, we discuss group-wise drugs. The GroupWise drugs are Antiulcer Drugs, Anti vomiting Drugs, Anti Inflammatory Drugs, Steroid Drugs, NSAID Drugs, Allergic Drugs, Pain Killer Drugs, Anti Asthmatic Drugs, Anthelmintic Drugs, Cardiovascular Drugs, Anti Hypertensive Drugs, Anti Cholesterol Drugs, Anti Platelet Drugs, Calcium Channel Blocker Drugs, Bronchodilator Drugs, Analgesic Antipyretic Drugs, Anti Vertigo Drugs, Anti Migraine Drugs, Antimicrobial Drugs, Antibiotic Drugs, Anti Bacterial Drugs, Anti Protozoal Drugs, Anti Fungal Drugs, Anti Viral Drugs, etc.
Great pharmacology topics range from core concepts (Pharmacokinetics/Dynamics, ANS, Receptors) to cutting-edge areas like Personalized Medicine (Pharmacogenomics), Antimicrobial Resistance, Neuropharmacology (Alzheimer’s, Pain), Cancer Pharmacology, Cardiovascular Drugs, and Drug Development/Discovery, focusing on specific diseases (e.g., Diabetes, TB, Malaria) or clinical issues like Pharmacovigilance, all offering deep dives into how drugs work, interact, and impact health.
Foundational & Core Topics
- Pharmacokinetics (PK) & Pharmacodynamics (PD): ADME (Absorption, Distribution, Metabolism, Excretion), Bioavailability, Half-life, Drug Interactions.
- Autonomic Nervous System (ANS): Cholinergic/Anticholinergic drugs, Adrenaline, Beta-blockers.
- Receptors: GPCRs, Ion Channels, Enzyme Inhibitors.
- Drug Discovery & Development: Clinical Trials, Novel Drug Delivery Systems (NDDS).
Hot & Advanced Topics
- Personalized Medicine: Pharmacogenomics (how genes affect drug response).
- Anti-Infectives: Antimicrobial Stewardship, Resistance (MRSA, TB), Antivirals, Antifungals.
- Neuropharmacology: Drugs for Epilepsy, Depression, Alzheimer’s, Parkinson’s, Opioids/Pain Management.
- Oncology (Cancer Drugs): Mechanisms, Resistance, Targeted Therapies.
- Cardiovascular: Anticoagulants (DOACs), Antiplatelets, Statins, Hypertension.
- Metabolic Disorders: Diabetes (Metformin, SGLT2i), Dyslipidemia.
Clinical & Applied Topics
- Pharmacovigilance: ADR Monitoring, Medication Safety, Drug Utilization Studies.
- Pharmacoeconomics: Cost-effectiveness, Quality of Life.
- Special Populations: Geriatric, Pediatric, Pregnancy Pharmacology.
- Ethnopharmacology: Herbal medicines, Natural Products.
How to Choose
- For Exams (High-Yield): Focus on core PK/PD, ANS, Autonomic Drugs, Antimicrobials, Cardiovascular (Anticoagulants/Antiplatelets), and CNS (Opioids, Antidepressants).
- For Projects/Research: Explore Pharmacogenomics, Personalized Medicine, Antimicrobial Resistance, Drug Delivery Systems, or specific disease management.
Study Of OTC Drugs for Best Paramedical Training Center In Bangladesh
The study of Over-The-Counter (OTC) drugs is a highly important topic due to their widespread use for self-care and minor ailments, which also presents significant public health challenges regarding misuse, potential adverse effects, and drug interactions.
Key Areas of Study
The most important topics within the study of OTC drugs include:
- Prevalence and Patterns of Self-Medication: Studies show a high prevalence of self-medication globally, ranging from 32.5% to over 80% in some populations. Analgesics (painkillers), cold and flu medications, and vitamins are among the most commonly used.
- Knowledge Gaps and Misconceptions: A significant public health concern is the lack of understanding among consumers, even among health science students, regarding proper use, dosage, side effects, and contraindications. For instance, many individuals incorrectly believe that antibiotics are OTC drugs.
- Safety and Associated Risks: Although generally considered safe when used as directed, OTC drugs are not risk-free.
- Misuse and Overdose: Taking higher-than-recommended doses, especially of active ingredients like acetaminophen or dextromethorphan (DXM), can lead to severe health effects, including liver damage or life-threatening reactions.
- Drug Interactions: OTC medications can interact with other prescription drugs, food, or alcohol, which can alter their effects and cause adverse outcomes.
- Masking Symptoms: Inappropriate use can mask the symptoms of underlying, more serious conditions, leading to delayed medical treatment.
- Influencing Factors: Consumer decisions are heavily influenced by convenience, desire to save time and money, prior experience, and information from family, friends, and mass media advertisements. The ease of access in community pharmacies and online platforms is a major factor in widespread use.
- Regulatory Framework and Education: Regulatory bodies like the FDA in the US ensure OTC products are safe and effective for self-use via specific monographs and clear “Drug Facts” labels. However, there is a continuous need for better public health education and stricter regulation of sales, especially online, to promote responsible self-medication practices.
- Specific Populations: Studies often focus on vulnerable populations such as adolescents, the elderly, or pregnant women, who may have unique risks or knowledge gaps related to OTC use.
Overall, the study of OTC drugs is vital for improving public health literacy and promoting the responsible use of these accessible medications to maximize their benefits while minimizing associated risks.
First Aid for Best Paramedical Training Center In Bangladesh
First Aid হলো কোনো ব্যক্তি অসুস্থ বা আহত হলে চিকিৎসক আসার আগে তাৎক্ষণিকভাবে দেওয়া প্রাথমিক সাহায্য।
এর মূল লক্ষ্য হলো –
- জীবন রক্ষা করা
- অবস্থা আরও খারাপ হওয়া থেকে রোধ করা
- দ্রুত আরোগ্যের সুযোগ সৃষ্টি করা
Objectives of First Aid
- Injured ব্যক্তির জীবন বাঁচানো
- রোগ বা আঘাতের অবনতি রোধ করা
- দ্রুত আরোগ্য লাভে সহায়তা করা
- রোগীকে হাসপাতালে পাঠানোর পূর্বে সঠিক যত্ন নেওয়া
Principles of First Aid
- Preserve life – রোগীর শ্বাস ও রক্ত সঞ্চালন বজায় রাখা
- Prevent further harm – আঘাতের অবস্থা খারাপ হতে না দেওয়া
- Promote recovery – ক্ষতস্থান পরিষ্কার, ব্যথা কমানো ও আরাম দেওয়া
- Seek medical help early – রোগীকে দ্রুত হাসপাতালে নেওয়া
Contents of First Aid Box
- Bandage (গজ, রোলার ব্যান্ডেজ)
- Cotton & Gauze
- Antiseptic (Dettol, Savlon, Spirit)
- Adhesive plaster
- Scissors & safety pins
- Thermometer
- Gloves
- Burn cream
- Pain killer (Paracetamol)
- ORS (Oral Rehydration Solution)
Common First Aid Procedures
1. Bleeding / Hemorrhage
- চাপ দিয়ে রক্ত বন্ধ করা
- পরিষ্কার কাপড় বা ব্যান্ডেজ ব্যবহার করা
- রোগীকে শান্ত রাখা
2. Burns & Scalds
- পোড়া স্থানে ঠান্ডা পানি ঢালা
- ফোস্কা না ফাটানো
- পোড়া স্থানে অয়েন্টমেন্ট লাগানো
3. Fracture (হাড় ভাঙা)
- রোগীকে নাড়াচাড়া না করা
- আক্রান্ত স্থানে স্প্লিন্ট দিয়ে স্থির করা
- হাসপাতালে পাঠানো
4. Shock
- রোগীকে সমতল স্থানে শোয়ানো
- পা কিছুটা উঁচু করে দেওয়া
- ঢিলেঢালা কাপড় পরানো
- দ্রুত চিকিৎসকের কাছে পাঠানো
5. Snake Bite
- কামড়ানো স্থানে টাইট ব্যান্ডেজ দেওয়া
- রোগীকে নাড়াচাড়া কম করতে দেওয়া
- বিষ চোষা নিষেধ
- হাসপাতালে নেওয়া
6. Fainting / Unconsciousness
- রোগীকে সমতল স্থানে শোয়ানো
- মাথা নিচু ও পা উঁচু রাখা
- বাতাস চলাচলের ব্যবস্থা করা
- পানি ছিটানো বা অ্যামোনিয়া ইনহেল করানো
7. Poisoning
- বমি করানো যাবে কি না তা বিষের ধরন অনুযায়ী (যেমন: এসিডে বমি করানো যাবে না)
- দ্রুত হাসপাতালে নিয়ে যাওয়া
8. CPR (Cardio Pulmonary Resuscitation)
- শ্বাস-প্রশ্বাস ও পালস নেই হলে
- 30 chest compression + 2 rescue breath
- অনবরত চালানো যতক্ষণ না সাহায্য আসে
Role of a Nurse in First Aid
- প্রাথমিক চিকিৎসা প্রদান
- রোগীকে শান্ত রাখা ও মানসিক সাপোর্ট দেওয়া
- রোগীর অবস্থা পর্যবেক্ষণ করা
- চিকিৎসকের নির্দেশ মতো ব্যবস্থা নেওয়া
- রোগীকে সঠিকভাবে হাসপাতালে রেফার করা
Hematology for Best Paramedical Training Center In Bangladesh
Important topics in Hematology cover blood cell formation (hematopoiesis), red blood cell disorders (anemias like iron deficiency, sickle cell, thalassemia), white blood cell/cancer (leukemia, lymphoma), bleeding/clotting issues (hemophilia, ITP, DIC), transfusion medicine, bone marrow issues, and diagnostic tools like CBC and smears, spanning both benign (classical) and malignant (oncology) conditions. Core areas include understanding normal blood physiology, common pathologies (anemias, malignancies, coagulation disorders), diagnostics (CBC, bone marrow biopsy), and treatments (transfusions, transplantation, gene therapy).
Core Concepts & Physiology
- Blood Composition: RBCs, WBCs, Platelets, Plasma, Proteins.
- Hematopoiesis: Bone marrow, stem cells, growth factors.
- Blood Cell Indices: MCV, MCHC, MCH, WBC differentials, ESR, Hematocrit.
- Hemostasis & Coagulation: Cascade, clotting factors, PT/aPTT, bleeding/clotting.
Benign (Classical) Hematology
- Anemias: Iron Deficiency, Megaloblastic (B12/Folate), Hemolytic (Sickle Cell, G6PD, Hereditary Spherocytosis), Aplastic Anemia, Thalassemia.
- Hemoglobinopathies: Sickle Cell Disease, Thalassemias (Alpha & Beta).
- Platelet Disorders: Thrombocytopenia, ITP (Immune Thrombocytopenic Purpura).
- Coagulation Disorders: Hemophilia, Von Willebrand Disease, DIC, Vitamin K deficiency.
Malignant Hematology (Hematology-Oncology)
- Leukemias: Acute (ALL, AML), Chronic (CML, CLL).
- Lymphomas: Hodgkin’s & Non-Hodgkin’s.
- Plasma Cell Disorders: Multiple Myeloma.
- Myeloproliferative Disorders & Myelodysplasia.
Diagnostics & Treatment
- Diagnostic Tools: CBC, Peripheral Blood Smear, Bone Marrow Biopsy/Aspiration, Coomb’s Test, Osmotic Fragility Test.
- Therapeutics: Blood Transfusions, Blood Banking, Chemotherapy, Stem Cell Transplant, Gene Therapy, Pharmacotherapy (Anticoagulants, Erythropoietin).
Key Conditions to Focus On
- Anemias: Iron Deficiency, Sickle Cell, Thalassemia, B12/Folate Deficiency.
- Malignancies: Leukemias, Lymphomas, Multiple Myeloma.
- Bleeding/Clotting: Hemophilia, ITP, DIC, Thrombosis.
- Transfusions: Reactions, blood banking principles.
Pathology for Best Paramedical Training Center In Bangladesh
Pathology plays a crucial role in medical practice by diagnosing diseases, advising on treatment, and monitoring patient conditions through laboratory tests and analysis of tissues and fluids. It is a bridge between science and medicine, providing the necessary diagnostic information for clinicians to make informed decisions. Pathologists, specialized medical professionals, analyze samples to identify the cause and nature of diseases, ultimately impacting patient care across various specialties.
Key Functions of Pathology in Medical Practice:
- Diagnosis:Pathologists help diagnose diseases by examining tissues, fluids, and cells, providing crucial information for determining the nature and cause of illness.
- Treatment Guidance:Pathology findings, such as identifying the type of cancer or the presence of an infection, guide treatment decisions, including the selection of appropriate medications, surgical interventions, or other therapies.
- Monitoring Patient Conditions:Pathology tests, like blood analysis or tissue biopsies, enable the monitoring of disease progression and the effectiveness of treatment, allowing for timely adjustments to patient care.
- Advancing Medical Knowledge:Pathology research and advancements in laboratory techniques contribute to a deeper understanding of diseases, leading to new diagnostic tools, treatments, and preventative measures.
Definition Pathology-Pathology is the study of diseases, their causes, mechanisms, structural and functional changes, and effects on the body.
Pathology হলো রোগের কারণ, প্রক্রিয়া, দেহের গঠন ও কাজের পরিবর্তন, এবং রোগের প্রভাব অধ্যয়নের বিজ্ঞান।
Objectives of Pathology
- Understand disease causes (etiology) – রোগের উৎপত্তি।
- Study pathogenesis – রোগ কীভাবে শরীরে প্রভাব ফেলে।
- Identify morphological changes – দেহের টিস্যু বা অঙ্গের পরিবর্তন।
- Guide diagnosis & treatment – চিকিৎসা ও নার্সিং পরিকল্পনায় সাহায্য।
Branches of Pathology
| Branch | English | Bangla |
|---|---|---|
| General Pathology | Study of disease mechanisms, cell injury, inflammation, tissue repair | রোগ প্রক্রিয়া, কোষ ক্ষতি, প্রদাহ, টিস্যু মেরামত অধ্যয়ন |
| Systemic Pathology | Study of specific organ systems & related diseases | নির্দিষ্ট অঙ্গ-প্রণালী ও সংশ্লিষ্ট রোগ অধ্যয়ন |
| Clinical Pathology | Laboratory study of blood, urine, body fluids | রক্ত, মূত্র, শরীরের তরল পরীক্ষার মাধ্যমে রোগ নির্ণয় |
| Surgical Pathology | Examination of tissues removed during surgery | অস্ত্রোপচারের সময় সরানো টিস্যুর পরীক্ষা |
Causes of Disease (Etiology)
- Genetic – Congenital diseases, Sickle cell anemia
- Infectious – Bacteria, Virus, Fungi, Parasites
- Environmental – Toxins, Radiation, Pollution
- Nutritional – Vitamin & mineral deficiency/excess
- Trauma / Physical injury – Burns, Fracture
Bangla:
রোগের কারণ হতে পারে বংশগত, সংক্রমণজনিত, পরিবেশজনিত, পুষ্টি জনিত, আঘাতজনিত।
Pathogenesis (Disease Mechanism)
- Disease process = How disease develops in body
- Example: Infection → Inflammation → Tissue damage → Symptoms
Bangla:
রোগের প্রক্রিয়া = রোগ কীভাবে শরীরে শুরু হয় ও টিস্যু ক্ষতি ঘটায়।
উদাহরণ: সংক্রমণ → প্রদাহ → টিস্যু ক্ষতি → লক্ষণ
Cell Injury & Death
- Reversible injury – Temporary damage (e.g., mild hypoxia)
- Irreversible injury / Cell death – Necrosis, Apoptosis
Bangla:
কোষ ক্ষতি: উল্টানোযোগ্য (অস্থায়ী), উল্টানো অসম্ভব (মৃত কোষ)
Inflammation (প্রদাহ)
- Acute – Short-term, redness, swelling, pain, heat
- Chronic – Long-term, tissue destruction, fibrosis
Bangla:
প্রদাহ = শরীরের প্রতিক্রিয়া সংক্রমণ বা আঘাতের প্রতি।
Acute = হঠাৎ, Chronic = দীর্ঘস্থায়ী
Tissue Repair (টিস্যু পুনরায় নির্মাণ)
- Regeneration – Damaged cells replaced by same type
- Repair / Scar formation – Fibrous tissue replaces lost cells
Bangla:
কোষ বা টিস্যু ক্ষতির পরে শরীরের পুনরায় গঠন বা দাগ তৈরি প্রক্রিয়া।
Disorders Common in Nursing
| Disease Type | English | Bangla | Nursing Focus |
|---|---|---|---|
| Blood Disorders | Anemia, Leukemia | রক্তের অসুখ | Monitor CBC, transfusion care |
| Infectious Diseases | TB, Malaria, Hepatitis | সংক্রমণজনিত রোগ | Infection control, isolation |
| Cardiovascular | Hypertension, MI | হৃদরোগ | Monitor vitals, medication |
| Respiratory | Pneumonia, Asthma | শ্বাসযন্ত্রের রোগ | Oxygen therapy, airway care |
| Metabolic | Diabetes, Thyroid disorder | পুষ্টি ও হরমোন জনিত রোগ | Blood sugar, medication |
| Renal | CKD, UTI | বৃক্কের রোগ | Fluid balance, urine monitoring |
Role of Nurse in Pathology
- Sample collection: Blood, urine, sputum
- Assist in lab tests & diagnosis
- Monitor patient condition & vitals
- Educate patient & family on disease
- Maintain infection control & hygiene
- Documentation & reporting
Cardiovascular Anatomy For Best Paramedical Training Center In Bangladesh
Important topics in cardiovascular anatomy include the heart’s structure (chambers, valves, layers, and great vessels), blood vessels (arteries, veins, capillaries), and the circulatory system (pulmonary and systemic circulation). Understanding the heart’s conduction system, cardiac cycle, and blood flow pathways is also crucial.
Detailed Breakdown:
1. The Heart:
- Chambers: Right atrium, left atrium, right ventricle, and left ventricle.
- Valves: Tricuspid, bicuspid (mitral), pulmonary, and aortic valves, ensuring unidirectional blood flow.
- Layers: Endocardium (inner), myocardium (muscle), and pericardium (outer protective layer).
- Great Vessels: Aorta, pulmonary artery, superior and inferior vena cava.
- Conduction System: Sinoatrial (SA) node, atrioventricular (AV) node, bundle of His, bundle branches, and Purkinje fibers, responsible for electrical impulses that regulate heartbeats.
2. Blood Vessels:
- Arteries: Carry oxygenated blood away from the heart (except for the pulmonary artery).
- Veins: Carry deoxygenated blood back to the heart (except for the pulmonary veins).
- Capillaries: Tiny vessels facilitating exchange of nutrients and waste between blood and tissues.
3. Circulatory System:
- Pulmonary Circulation: The flow of blood between the heart and lungs for oxygenation.
- Systemic Circulation: The flow of blood from the heart to the rest of the body and back.
4. Other Important Aspects:
- Cardiac Cycle: The sequence of events during one heartbeat, including atrial and ventricular contractions and relaxations.
- Blood Pressure: The force exerted by blood against the walls of blood vessels, regulated by factors like baroreceptors and the renin-angiotensin-aldosterone system.
- Coronary Circulation: The blood supply to the heart muscle itself.
- Age-related changes: Physiological changes in the cardiovascular system with age.
Neuro Anatomy & Physiology for Best Paramedical Training Center In Bangladesh
Neuro anatomy and Physiology is a foundational subject in medical and neuroscience fields, covering essential topics that explain the structure and function of the body’s control center. Mastery of these areas is crucial for understanding how the body maintains homeostasis and for diagnosing and treating neurological disorders.
Key Neuroanatomy Topics
- Divisions of the Nervous System: Understanding the organization into the Central Nervous System (CNS) (brain and spinal cord) and the Peripheral Nervous System (PNS) (all other nerves).
- Major Brain Structures: The anatomy and function of the cerebrum, cerebellum, brainstem (midbrain, pons, medulla oblongata), diencephalon (thalamus and hypothalamus), basal ganglia, and limbic system.
- Spinal Cord and Tracts: The structure of the spinal cord, its segments, and the major ascending (sensory) and descending (motor) tracts (e.g., corticospinal, spinothalamic tracts).
- Meninges and Cerebrospinal Fluid (CSF): The protective coverings of the brain and spinal cord and the circulation and function of the CSF.
- Vascular Supply: The blood supply to the brain, including the vital Circle of Willis, and the concept of the blood-brain barrier.
- Cranial Nerves: The 12 pairs of cranial nerves, their origins, functions (sensory, motor, or mixed), and clinical correlations.
- Embryology: The basic development of the nervous system (neurulation, formation of the neural tube) to understand congenital anomalies.
Key Neurophysiology Topics
- Neuronal Signaling: The mechanisms of nerve impulse transmission, including the resting membrane potential, action potentials, and synaptic transmission.
- Neurotransmitters: The types and roles of key chemical messengers (e.g., acetylcholine, dopamine, serotonin, glutamate, GABA) in modulating mood, cognition, and movement.
- Motor Control: The physiological processes by which voluntary movements are planned and executed, involving the motor cortex, basal ganglia, and cerebellum.
- Autonomic Nervous System (ANS): The function of the sympathetic (“fight-or-flight”) and parasympathetic (“rest-and-digest”) divisions and how they regulate involuntary functions like heart rate and digestion.
- Sensory Physiology: The mechanisms of general senses (touch, pain, temperature, proprioception) and special senses (vision, hearing, balance, smell, taste).
- Higher Brain Functions: The physiological basis of complex functions such as consciousness, memory, learning, emotion, and sleep.
- Homeostasis and Reflexes: The role of the nervous system, particularly the hypothalamus and brainstem, in maintaining a stable internal environment and coordinating essential reflexes (e.g., breathing, heart rhythm).
These topics provide a comprehensive understanding of how the nervous system coordinates the body’s activities and responds to stimuli. Reputable sources like Johns Hopkins Medicine and the National Institutes of Health (NIH) offer in-depth information on these subjects.
Surgery For Best Paramedical Training Center In Bangladesh
Key surgery topics include trauma, gastrointestinal surgery (including colorectal, hepatobiliary, and pancreatic), wound healing, and perioperative care. Other very important subjects are surgical infections, basic surgical principles, breast and endocrine surgery, and various aspects of patient safety and management.
Core subjects
- Basic principles: Fundamental concepts that apply across all surgical procedures.
- Wound healing: Understanding the processes of tissue repair and complications like infection.
- Perioperative care: Management of patients before, during, and after surgery, including anesthesia and post-operative care.
- Surgical infections: Knowledge of infections, such as MRSA, and their prevention and treatment.
- Trauma: Management of traumatic injuries.
System-specific subjects
- Gastrointestinal surgery: Includes topics like inflammatory bowel disease (Crohn’s and ulcerative colitis), gallstones, and pancreatitis.
- Hepatobiliary and pancreatic surgery: Focuses on the liver, gallbladder, and pancreas.
- Colorectal surgery: Deals with the colon and rectum.
- Breast and endocrine surgery: Covers breast cancer and conditions like thyroid and adrenal tumors.
- Vascular and endovascular surgery: Involves blood vessels and includes both surgical and less invasive endovascular techniques.
- Cardiothoracic surgery: Covers the heart and lungs.
- Plastic and reconstructive surgery: Includes burns and other skin-related issues.
Patient and procedural management
- Patient safety: Protocols and technologies to ensure patient safety during surgery.
- Oncology: The surgical management of cancer.
- Diagnosis and intervention: Includes history, examination, diagnostic studies, and surgical interventions.
- Pharmacotherapy: Use of drugs in a surgical context.
- Emergency medicine: Management of surgical emergencies.
- Bariatric surgery: Procedures for managing obesity.
Medical Diagnosis For Best Paramedical Training Center In Bangladesh
medical diagnosis include understanding various disease categories, diagnostic procedures, and the evolving nature of diagnosis itself, with a focus on both accuracy and timeliness. Key areas involve recognizing critical conditions early, leveraging diagnostic tests effectively, and staying abreast of advancements like AI in diagnostics.
Key Areas in Medical Diagnosis:
Understanding Disease Categories: Medical diagnosis relies on recognizing and categorizing diseases. This includes understanding cancers, diabetes, infections, mental health conditions, and more.
Diagnostic Procedures: Various tests and procedures are used, including blood tests (like CBC), imaging (X-rays, ultrasound, etc.), biopsies, and more.
Timeliness and Accuracy: Accurate and timely diagnosis is crucial, as delays or misdiagnoses can lead to harm.
Evolution of Diagnosis: The field of diagnosis is constantly evolving, with new technologies and approaches emerging, like AI in medical diagnostics.
Ethical Considerations: The diagnostic process also involves ethical considerations, such as avoiding overdiagnosis and ensuring patient safety.
Medical Biochemistry For Best Paramedical Training Center In Bangladesh
Medical Biochemistry include carbohydrate, lipid, and protein metabolism, along with molecular biology and genetics. These are fundamental to understanding how the body functions at a cellular and molecular level, and they are crucial for various medical applications.
Important Topics :
1. Metabolism:
Carbohydrate Metabolism: Glycolysis, gluconeogenesis, the citric acid cycle (TCA cycle), glycogen metabolism (glycogenesis, glycogenolysis), and the pentose phosphate pathway are essential for energy production and glucose homeostasis.
Lipid Metabolism: Beta-oxidation of fatty acids, ketone body synthesis and utilization, cholesterol synthesis, and lipoprotein metabolism are vital for understanding energy storage and transport.
Protein and Amino Acid Metabolism: Amino acid biosynthesis and degradation, protein turnover, and the urea cycle are important for understanding protein synthesis and nitrogen balance.
2. Molecular Biology:
DNA Replication, Transcription, and Translation: Understanding these processes is crucial for gene expression and protein synthesis.
Genetic Code: Knowledge of codons, anticodons, and the genetic code is fundamental for understanding how genetic information is translated into proteins.
3. Cellular Processes:
Enzymology: Enzyme kinetics, mechanisms of enzyme action, and enzyme regulation are essential for understanding how biochemical reactions are catalyzed.
Cellular Respiration: Oxidative phosphorylation and the electron transport chain are crucial for ATP production.
Membrane Transport: Understanding how molecules move across cell membranes is crucial for cellular function and homeostasis.
4. Other Important Areas:
Vitamins and Minerals: Understanding the role of vitamins and minerals as cofactors for enzymes and their importance in various metabolic pathways.
Hormonal Regulation: Understanding how hormones regulate metabolism and other cellular processes.
Clinical Biochemistry: Understanding how biochemical markers are used to diagnose and monitor diseases.
Inborn Errors of Metabolism: Understanding the genetic basis of these diseases and their impact on metabolism.
Free Radicals and Antioxidants: Understanding the role of free radicals in oxidative stress and the importance of antioxidants in protecting against cellular damage.
By focusing on these key areas, medical students can build a strong foundation in biochemistry and prepare themselves for success in their studies and future medical careers.
Orthopedic Anatomy For Best Paramedical Training Center In Bangladesh
Orthopedic anatomy include bone and joint structure, fracture types and healing, muscle and tendon attachments, nerve and blood supply, and common orthopedic conditions like arthritis, osteoporosis, and spinal disorders. Understanding the biomechanics of joints, recognizing common injuries, and knowing the basics of fracture management are crucial.
1. Bone and Joint Anatomy:
- Bone Structure: Types of bone (compact, spongy), bone cells, bone matrix, bone marrow, and bone circulation.
- Joint Structure: Types of joints (fibrous, cartilaginous, synovial), joint capsules, ligaments, and articular cartilage.
- Specific Joints: Knee, hip, shoulder, elbow, and ankle joints, including their bony structures, ligaments, and surrounding muscles.
- Lower Limb: Femoral triangle, popliteal fossa, sciatic nerve, arches of the foot, and venous drainage.
- Upper Limb: Brachial plexus, axilla, elbow, wrist, and hand.
- Spine: Vertebral column, spinal cord, intervertebral discs, and spinal ligaments.
2. Fractures and Healing:
- Fracture Types: Salter-Harris classification, fracture patterns, and open vs. closed fractures.
- Fracture Healing: Stages of fracture healing, factors affecting healing, and potential complications like nonunion.
- Specific Fracture Sites: Clavicle, humerus, femur, tibia, fibula, scaphoid, and other common fracture locations.
3. Muscle and Tendon Anatomy:
- Muscle Attachments: Origin and insertion points of major muscles, especially those involved in joint movements.
- Tendon Function: Role of tendons in connecting muscles to bones and transmitting forces.
- Muscle Physiology: Basic muscle contraction and relaxation mechanisms.
4. Nerve and Blood Supply:
- Peripheral Nerves: Radial, ulnar, median, sciatic nerves, and their distributions.
- Blood Supply: Arterial supply to the limbs and the potential for vascular compromise in certain injuries.
5. Common Orthopedic Conditions:
- Arthritis: Osteoarthritis, rheumatoid arthritis, and other types, including their clinical presentation and management.
- Osteoporosis: Bone density loss, risk factors, and prevention strategies.
- Spinal Disorders: Disc prolapse, spinal stenosis, and spondylolisthesis.
- Other Conditions: Osteomyelitis, bone tumors, congenital hip dislocation, and compartment syndrome.
6. Biomechanics:
- Joint Biomechanics: How joints move and how forces are distributed across them.
- Gait Analysis: Understanding the biomechanics of walking and running.
- Orthopedic Implants: Basic principles of implant design and function.
7. Imaging and Diagnostics:
- Radiological Features: Understanding common radiographic findings in orthopedic conditions.
- MRI and CT Scans: Use and interpretation of these imaging modalities in orthopedics.
8. Surgical Procedures:
- Basic surgical principles: Wound management, anesthesia, and asepsis.
- Common orthopedic procedures: Fracture fixation, joint replacement, arthroscopy, and soft tissue repairs.
- Rehabilitation: Principles of post-operative care and physical therapy.
This list provides a comprehensive overview of important topics in orthopedic anatomy. Remember to focus on the clinically relevant aspects of each topic, as this will be most useful in practical applications.
Practical Class on Heartbeat for Best Paramedical Training Center In Bangladesh
A heartbeat is the rhythmic contraction and relaxation of the heart, driven by electrical signals, pumping blood through the body; it involves phases like diastole (relaxation/filling) and systole (contraction/pumping) and is measured as beats per minute (BPM), with 60-100 BPM being a normal resting range for adults, though it varies with activity. The electrical impulse originates at the sinoatrial (SA) node, travels through the atria, and then to the ventricles, causing them to contract and pump oxygenated and deoxygenated blood.
How it works (The Cardiac Cycle)
- Diastole (Relaxation): The heart’s chambers relax, and blood flows from the body into the right atrium and from the lungs into the left atrium, then into the ventricles.
- Atrial Systole: The atria contract, pushing remaining blood into the ventricles.
- Ventricular Systole: The ventricles contract forcefully, pushing blood out: the right side sends it to the lungs, and the left side pumps it to the rest of the body.
- Cycle Repeats: The heart then re-enters diastole, refilling with blood.
Key Terms
- SA Node: The heart’s natural pacemaker, initiating the electrical signal.
- Pulse: The palpable wave of blood flow from the heart’s beat.
- Heart Rate: The number of beats per minute (BPM).
- Tachycardia: A heart rate over 100 BPM at rest.
- Bradycardia: A slow heart rate (not mentioned in snippets, but implied opposite of tachycardia).
What affects it
- Factors Such as Stress, caffeine, nicotine, exercise, and hormones can increase heart rate.
- Normal Range: 60-100 BPM at rest for most adults, though athletes often have lower rates.
Practical Class on Heart Rate for Best Paramedical Training Center In Bangladesh
Heart rate is the number of times your heart beats per minute (bpm), with a normal resting rate for adults generally being 60-100 bpm, though it varies with age, fitness, stress, and medications, with athletes often having lower rates. It’s a key health indicator, reflecting heart function; a consistently high rate (tachycardia, >100 bpm at rest) or low rate (bradycardia, <60 bpm at rest, unless fit) can signal issues. You can check it by feeling your pulse at the wrist or with devices, ideally after resting.
Normal Ranges & Factors
- Adults: 60-100 bpm resting.
- Athletes: Can be as low as 40 bpm or less.
- Children: Have higher rates, e.g., 80-120 bpm for ages 3-5.
- Factors Affecting It: Fitness, emotions, caffeine, alcohol, medications, illness, pregnancy, and sleep quality.
How to Check Your Heart Rate
- Rest: Sit quietly for 5-10 minutes.
- Locate Pulse: Place index and middle fingers on the thumb side of your wrist.
- Count: Count beats for 15 seconds and multiply by 4, or count for a full minute.
- Devices: Smartwatches and fitness trackers offer easy monitoring.
Practical Class on Inhaler & Rotahaler for Best Paramedical Training Center In Bangladesh
A practical class on inhalers and Rotahalers should focus on ensuring correct administration technique, as proper use is crucial for the medication to reach the lungs effectively.
The main important topics for a practical class include:
General Inhaler Principles
- Mechanism of Action: Understanding how inhaled medication directly targets the lungs to control conditions like asthma and COPD, and the advantages over systemic therapy.
- Importance of Correct Technique: Highlighting that poor technique is a major cause of poor disease control, and little or no medicine reaches the lungs if used incorrectly.
- Types of Inhalers: Distinguishing between different types, such as metered-dose inhalers (MDIs), dry powder inhalers (DPIs, which include the Rotahaler), and soft mist inhalers (SMIs), and when each might be appropriate for different patients.
- Common Errors: Identifying frequent mistakes, such as not exhaling fully before inhalation or not holding one’s breath afterwards.
- Patient Education: Emphasizing the need for healthcare providers to give clear verbal and demonstrated instruction, and observe the patient re-demonstrate the technique at each visit.
Specific Inhaler Technique Steps
The practical component should cover the step-by-step procedures for each device.
For Rotahaler (Dry Powder Inhaler)
- Preparation:
- Unscrew the cover and hold the Rotahaler vertically.
- Insert the capsule (Rotacap) correctly into the chamber, ensuring the clear end is in the smaller hole.
- Press the capsule firmly and rotate the base of the device to pierce and open the capsule.
- Inhalation:
- Breathe out gently and fully, away from the device.
- Place the mouthpiece in the mouth, sealing lips around it.
- Breathe in deeply and forcefully to ensure the powder is inhaled into the lungs.
- Remove the device from the mouth and hold the breath for at least 10 seconds, or as long as comfortable.
- Post-use Care:
- Check the chamber to confirm the capsule is empty.
- Discard the empty capsule shell.
- Discuss the importance of cleaning the Rotahaler and how often (e.g., every two weeks).
- Crucial Step for Steroids: If the medication is a corticosteroid, rinse or gargle the mouth with plain water and spit it out to prevent oral thrush.
For Pressurized Metered-Dose Inhaler (pMDI)
- Preparation:
- Remove the cap and shake the inhaler well before use.
- If a spacer is available, attach it, especially for patients who struggle with coordination.
- Inhalation:
- Breathe out fully, away from the inhaler.
- Place the mouthpiece in the mouth, or into the spacer.
- As the patient starts to breathe in slowly and steadily, press down on the canister to release the medication.
- Continue breathing in, then hold the breath for 5 to 10 seconds.
- Post-use Care:
- If multiple puffs are needed, wait as advised by the manufacturer/pharmacist before repeating the steps.
- Clean the MDI regularly (e.g., once a week with warm water).
- Rinse mouth after use if it contains a steroid.
Practical Class on Tachycardia for Best Paramedical Training Center In Bangladesh
Tachycardia is a heart rhythm disorder where the heart beats too fast, typically over 100 beats per minute (bpm) at rest in adults, signaling an electrical problem or normal response to stress, exercise, or underlying conditions like fever, anemia, anxiety, or thyroid issues, causing symptoms like palpitations, dizziness, and shortness of breath, requiring medical evaluation to determine if it’s benign (sinus tachycardia) or a serious arrhythmia needing treatment.
Types of Tachycardia
- Sinus Tachycardia: A normal response to stress, fever, or exercise, where the sinus node fires too quickly.
- Supraventricular Tachycardia (SVT): Abnormal signals start above the ventricles, causing sudden, rapid heartbeats, often felt as palpitations.
- Ventricular Tachycardia (VT): A dangerous rhythm originating in the heart’s lower chambers, potentially life-threatening.
- Atrial Fibrillation (AFib) & Flutter: Irregular, rapid heartbeats in the upper chambers (atria).
Common Symptoms
Racing heart or palpitations, Dizziness or lightheadedness, Shortness of breath, and Chest pain or discomfort.
Common Causes & Triggers
- Lifestyle: Caffeine, alcohol, stimulants, smoking, stress, lack of sleep.
- Medical Conditions: Fever, anemia, thyroid disease, dehydration, lung disease, sleep apnea, heart disease, and high blood pressure.
- Electrical Issues: Faulty heart wiring or triggers in the heart’s chambers.
Practical Class on Bradycardia for Best Paramedical Training Center In Bangladesh
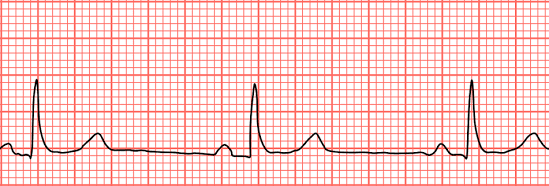

Bradycardia is a slower-than-normal heart rate, typically under 60 beats per minute (bpm) in adults at rest, caused by issues with the heart’s electrical system, certain medications, or underlying conditions like sleep apnea or thyroid problems, leading to symptoms like dizziness, fatigue, shortness of breath, and confusion, though highly fit individuals and athletes may have a normal slow rate. Treatment varies by cause, ranging from lifestyle changes to pacemakers, and involves diagnosing the underlying problem with tools like an EKG.
What it is
- A heart rate below 60 bpm, meaning the heart isn’t pumping enough oxygen-rich blood to the body.
- Can be normal for athletes or during sleep, but problematic if it causes symptoms.
Common types
- Sinus Bradycardia: Slowing of the heart’s natural pacemaker (sinus node).
- Heart Block: Electrical signals from the upper to lower heart chambers are blocked.
Causes
- Heart Issues: Heart disease, previous heart attacks, sick sinus syndrome.
- Medications: Beta-blockers, calcium channel blockers.
- Medical Conditions: Thyroid problems, electrolyte imbalances, sleep apnea, and inflammation.
- Lifestyle: Intense physical fitness (often normal), aging.
Symptoms (when problematic)
- Dizziness, lightheadedness, fainting.
- Fatigue, weakness.
- Shortness of breath, chest pain.
- Confusion or memory problems.
Diagnosis & Treatment
- Diagnosis: Physical exam, EKG, Holter monitor, sleep study, blood tests.
- Treatment: Addressing the cause (e.g., changing meds, treating sleep apnea) or using a pacemaker for severe cases.
Practical Class on IM Injection Pushing for Best Paramedical Training Center In Bangladesh
The process of pushing an intramuscular (IM) injection involves a smooth, steady depression of the plunger after the needle is securely in the muscle, ensuring the medication goes in slowly to minimize discomfort, followed by quickly withdrawing the needle at the same angle and activating the safety device, then applying gentle pressure to the site with gauze. Key steps include site preparation (cleaning, Z-track method), swift 90-degree needle insertion, slow plunger push (counting to three), quick withdrawal, and immediate disposal in a sharps container.
Pre-Injection Steps (Preparation)
- Hand Hygiene & Supplies: Wash hands thoroughly and gather medication, syringe, alcohol swabs, gauze, and a sharps container.
- Site Selection & Prep: Locate the correct muscle (e.g., deltoid, ventrogluteal), clean with an alcohol swab, and let it dry.
- Z-Track Method (Optional but Recommended): Use your non-dominant hand to pull the skin and tissue to the side to prevent medication leakage into subcutaneous tissue.
- Syringe Prep: Remove the cap, ensure no large air bubbles, and tap to get a drop of medication at the tip.
The “Push” (Injection)
- Insertion: Hold the syringe like a dart and insert the needle quickly at a 90-degree angle into the muscle.
- Stabilize: Once in the muscle, use your non-dominant hand to steady the syringe.
- Depress Plunger: Slowly and steadily push the plunger all the way down, counting to three.
- Withdrawal: After the fluid is in, hold for a few seconds (around 10 for some meds), then pull the needle straight out at the same 90-degree angle.
Post-Injection Steps
- Safety: Immediately activate the needle’s safety shield and dispose of the entire syringe in the sharps container.
- Site Care: Apply gentle pressure with gauze or a cotton ball (no rubbing) and secure with a bandage if needed.
- Observe: Monitor the patient for any adverse reactions.
Process of IV Injection Pushing in Best Paramedical Training Center In Bangladesh
The process of IV Injection Pushing (or Bolus) involves a trained healthcare professional manually injecting medication directly into an established IV line using a syringe, following strict steps: verify order, prepare patient, scrub the IV port (clave), flush with saline to check for patency, attach the medication syringe, push the drug at a specific rate (seconds to minutes) while monitoring, and then perform a post-flush to clear the line, ensuring patient safety and proper delivery.
Key Steps in IV Push Administration
- Preparation & Verification:
- Confirm the doctor’s order, patient details, medication rights (right drug, dose, time, route, patient, documentation, reason, response).
- Gather supplies: saline flush, medication syringe, alcohol wipes, and gloves.
- Perform hand hygiene and don gloves.
- Educate the patient about the medication and potential side effects.
- Priming & Flushing (SASH Method):
- Saline Flush: Scrub the injection port (clave) with an alcohol wipe for 15-30 seconds, let it air dry, then inject 3-5mL of saline to check for patency (blood return) and clear the line.
- Medication Administration:
- Attach Medication: Attach the pre-filled medication syringe (air expelled) to the scrubbed port and twist clockwise to secure.
- Slow Push: Slowly inject the medication at the prescribed rate (e.g., over 1 minute, 2 minutes). Use a timer for accuracy; break down the volume into smaller intervals for easier pacing (e.g., 0.5mL every 30 seconds for a 1mL/min push).
- Completion (SASH):
- Follow-up Flush: After the medication, flush with another 3-5mL of saline at the same rate as the medication push to ensure all the drug enters the bloodstream and clears the tubing, preventing incompatibility with other IV fluids.
- Secure the port with a new alcohol cap if required by facility policy.
Important Considerations
- Timing is Crucial: Pushing too fast can cause adverse effects or medication waste; too slow might delay treatment.
- Compatibility: Always check if the medication is compatible with the primary IV fluid running, if any.
- Patient Monitoring: Closely watch the patient for any adverse reactions during and after administration, especially respiratory changes, notes LevelUpRN.
Practicle Class on Pulse Measurement for Best Paramedical Training Center In Bangladesh
The most important topics for a practical class on pulse measurement involve understanding the parameters of the pulse (rate, rhythm, and force), the technique of palpation, various pulse points, and factors influencing the reading.
Key Learning Objectives & Topics
- Anatomy and Physiology:
- Understand what pulse is (the rhythmic expansion and recoil of an artery as blood is pumped through it) and how it relates to the heartbeat (heart rate).
- Identify the major arteries used for pulse measurement (e.g., radial, carotid, brachial, femoral, etc.) and their locations.
- Measurement Technique (Palpation):
- Proper hand hygiene and patient preparation (consent, ensuring the patient is relaxed).
- Correct finger placement (using index and middle fingers, not the thumb).
- Applying appropriate pressure to feel the pulse clearly without blocking blood flow.
- Counting method: Measuring for a full 60 seconds (especially if irregular) or 30 seconds and multiplying by two if regular.
- Parameters of the Pulse:
- Rate: Normal ranges for different age groups (e.g., 60-100 bpm for healthy adults).
- Rhythm: Assessing if the beats are regular (even tempo) or irregular (regularly irregular or irregularly irregular).
- Force/Volume (Strength): Subjectively grading the pulse strength (e.g., weak/thready, normal/strong, bounding) using a scale.
- Bilateral Equality: Comparing pulses on both sides of the body (e.g., both radial pulses) to check for potential circulatory issues like arterial obstructions.
- Factors and Abnormalities:
- Discussing factors that can influence pulse rate (physical activity, emotions, age, medications, temperature, health conditions).
- Recognizing and recording abnormal findings (e.g., tachycardia, bradycardia, weak pulse in shock) and their potential clinical significance.
- Documentation:
- Accurately recording the pulse rate, rhythm, and strength in patient notes.
Practical Application
Students should practice finding and assessing pulses at various points, with the radial artery being the most common site for routine checks. The carotid pulse is important for emergency assessment, but students must learn never to palpate both carotid arteries simultaneously to avoid reducing blood flow to the brain.
Practicle Class on Nebulizer for Best Paramedical Training Center In Bangladesh
A practical class on nebulizers typically covers both the theoretical knowledge and the hands-on skills needed for safe and effective use. Main important topics are centered around understanding the device, proper administration technique, patient safety, and hygiene protocols.
Key Topics for a Practical Nebulizer Class
A practical class is likely to cover the following essential topics:
1. Theory and Indications
- Definition and Function: Understanding how a nebulizer converts liquid medication into a fine mist (aerosol) that can be inhaled deep into the lungs.
- Indications for Use: Identifying which respiratory conditions, such as asthma or COPD, require nebulization therapy.
- Types of Nebulizers: Distinguishing between different types (jet, ultrasonic, mesh) and their respective advantages, disadvantages, and appropriate applications.
- Medications: Learning about the various types of medications (e.g., bronchodilators, corticosteroids, mucolytics) that can be administered via nebulizer and their effects.
2. Procedure and Technique
- Preparation: Assembling the equipment (compressor, tubing, medication cup, mask/mouthpiece) and preparing the correct dose of medication.
- Patient Positioning: Ensuring the patient is in a comfortable, upright position (sitting or semi-Fowler’s) to enable maximum breathing efficiency.
- Administration Steps: A step-by-step guide to delivering the treatment effectively, including using a mouthpiece or mask correctly and encouraging slow, deep breaths through the mouth.
- Monitoring: Observing the patient during treatment for signs of improvement or adverse reactions such as palpitations, tremors, or increased difficulty breathing.
3. Safety and Maintenance
- Infection Control: Emphasizing stringent hygiene practices, including washing hands before and after treatment, and the importance of using single-use or personal equipment to prevent cross-infection.
- Cleaning and Disinfection: Proper disassembly, cleaning with soapy water, rinsing, and thorough drying of reusable parts after each use to prevent microbial growth.
- Troubleshooting: Identifying and resolving common issues, such as the machine not producing mist or unusual noises.
- Special Considerations: Adjusting the procedure for specific patient populations, such as infants, young children, or unconscious patients who may require a face mask or alternative positioning.
4. Documentation and Education
- Record Keeping: Accurately documenting the procedure, administered medication, dosage, time, and the patient’s response in their care plan or medical record.
- Patient Teaching: Instructing patients and caregivers on proper home use, maintenance, and when to report symptoms to a physician to ensure compliance and effective long-term management.
Practicle Class on Saline Infusion for Best Paramedical Training Center In Bangladesh
A practical class on saline infusion focuses on the core principles and procedures of intravenous fluid administration. Key topics include the indications and contraindications for use, the types of saline solutions, and the essential practical skills for administration and patient monitoring.
Core Topics for a Practical Class
1. Foundational Knowledge and Principles
- Physiology of Fluid Balance: Understanding how water and electrolytes are distributed and balanced in the body is crucial for safe fluid therapy.
- Types of IV Fluids: Differentiating between isotonic (e.g., 0.9% Normal Saline), hypotonic (e.g., 0.45% Saline), and hypertonic solutions based on their osmolarity and clinical use.
- Indications for Saline Infusion: Common uses for normal saline (0.9% NaCl) include:
- Extracellular fluid replacement (dehydration, hypovolemia, hemorrhage, sepsis).
- Treatment of metabolic alkalosis.
- Mild sodium depletion.
- Vehicle for diluting and administering compatible medications.
- Administering blood products.
- Contraindications and Cautions: Identifying conditions where saline infusion should be used with caution or avoided, such as congestive heart failure, severe renal impairment, or conditions involving sodium retention due to the risk of fluid volume overload.
2. Equipment and Preparation
- Identifying Supplies: Recognizing and preparing all necessary equipment, including IV bags, administration sets (tubing), IV cannula/catheter, tourniquet, antiseptic solution, and sterile gloves.
- Aseptic Technique: Emphasizing the mandatory use of sterile techniques throughout the procedure to prevent infection.
- Preparing the Solution and Tubing:
- Checking the IV fluid for clarity, expiry date, and any signs of contamination.
- Spiking the IV bag and priming the tubing to remove all air bubbles and prevent air embolism.
- Proper labeling of the IV bag and tubing with medication (if added), date, time, and flow rate.
3. Administration Procedure and Skills
- Patient Preparation: Explaining the procedure to the patient, obtaining consent, and ensuring a comfortable position.
- Venipuncture: Selecting an appropriate vein and inserting the IV cannula correctly.
- Calculating and Regulating Flow Rate: Learning how to manually calculate the drip rate or use an infusion pump to ensure the correct volume is delivered over the specified time.
- Troubleshooting: Addressing potential issues, such as an insufficient flow rate, pain at the injection site, or equipment failure.
4. Monitoring and Management
- Patient Monitoring: Continuously assessing the patient for signs of adverse reactions or complications, including:
- Local reactions: Pain, swelling, redness, phlebitis, or extravasation at the injection site.
- Systemic reactions: Fluid overload (peripheral/pulmonary edema, high blood pressure), electrolyte imbalances (hypernatraemia, hyponatraemia), or systemic infection.
- Documentation: Accurately recording the procedure details, including the type and amount of fluid/medication administered, flow rate, and patient response.
- When to Discontinue: Understanding the criteria for stopping the infusion and when to seek senior medical advice, especially in cases of adverse events.
Practicle Class on cannula for Best Paramedical Training Center In Bangladesh
A practical class on intravenous (IV) cannulation should focus on both theoretical knowledge and the hands-on skills required for safe and effective practice.
Key Theoretical Topics
- Anatomy and Physiology: Understanding the circulatory system, including differentiating between veins and arteries, and identifying suitable peripheral veins for cannulation (e.g., in the forearm, back of the hand).
- Indications and Contraindications: Knowing when IV access is necessary (e.g., for fluid administration, medication, blood transfusions, or drawing blood samples) and when it might be contraindicated (e.g., in an arm with an AV fistula or a history of breast surgery/lymph node removal).
- Cannula Selection: Learning about the different cannula sizes (gauges), their corresponding flow rates, and selecting the appropriate size based on the patient’s needs and vein condition.
- Infection Prevention and Control: Emphasizing the importance of strict aseptic non-touch technique (ANTT) to minimize the risk of infection.
- Potential Complications: Recognizing, preventing, and managing common complications such as hematoma, phlebitis, infiltration/extravasation (fluid leaking into surrounding tissue), and accidental arterial puncture.
- Documentation and Aftercare: Understanding the correct procedures for labeling the cannula site with the date/time of insertion and documenting the procedure in the patient’s records.
Essential Practical Skills
- Patient Preparation and Consent: Effectively explaining the procedure to the patient, confirming their identity, obtaining informed consent, and ensuring their comfort.
- Equipment Preparation: Assembling all necessary equipment (cannula, tourniquet, antiseptic wipes, dressing, saline flush, gloves, sharps bin) in an organized manner.
- Vein Selection and Preparation:
- Applying a tourniquet correctly.
- Identifying and palpating a suitable vein.
- Cleaning the chosen site with an antiseptic solution and allowing it to air dry.
- Insertion Technique:
- Stabilizing the vein by applying traction to the skin.
- Inserting the cannula (bevel up) at a shallow angle.
- Observing for “flashback” of blood to confirm venous entry.
- Advancing the cannula into the vein while retracting the needle (stylet) safely into its protective mechanism.
- Securing and Flushing:
- Releasing the tourniquet.
- Connecting the bionector/T-piece and flushing the cannula with saline to check for patency and signs of infiltration.
- Securing the cannula firmly with an appropriate sterile dressing, ensuring the insertion site remains visible for monitoring.
- Removal of Cannula: Learning the correct procedure for safely removing the cannula when it is no longer needed or if complications arise.
For visual examples of the procedure and equipment, you can refer to online resources and training materials (e.g., TeachMeSurgery, Ausmed).
Practicle Class on Oxygen Measurement for Best Paramedical Training Center In Bangladesh
A practical class on oxygen measurement covers different topics depending on whether the focus is on chemistry/environmental science (measuring oxygen in a lab or water) or biomedical/clinical science (measuring oxygen in the body).
For Biomedical/Clinical Context
The main important topics for a practical class on measuring oxygen in a clinical or physiological setting include:
- Physiology of Oxygen Transport: Understanding how oxygen is absorbed by the lungs and transported in the blood, primarily bound to hemoglobin.
- Oxygen Saturation (SpO₂) and Partial Pressure (PO₂): Defining and distinguishing between oxygen saturation (the percentage of hemoglobin carrying oxygen) and the partial pressure of oxygen in arterial blood.
- Pulse Oximetry: The core practical skill, covering the principles (spectrophotometry and light absorption differences between oxygenated and deoxygenated hemoglobin), proper use of a pulse oximeter, and factors affecting accuracy (e.g., patient movement, nail polish, tissue thickness).
- Blood Gas Analysis (BGA): An invasive but highly accurate method that provides comprehensive information, including arterial oxygen saturation (SaO₂), partial pressure of oxygen (PaO₂), pH, and carbon dioxide levels.
- Clinical Significance: Interpreting results, recognizing normal ranges (typically 95-99% SpO₂), identifying hypoxemia (low blood oxygen levels), and understanding the need for medical interventions like oxygen therapy.
- Oxygen-Hemoglobin Dissociation Curve: Understanding the relationship between PO₂ and oxygen saturation and how factors like pH and temperature shift this curve.
For Chemistry/Environmental Science Context
The main important topics for a practical class on measuring oxygen in a laboratory or environmental setting include:
- Chemical Test for Gaseous Oxygen: Performing the standard qualitative test using a glowing splint which relights in the presence of oxygen.
- Preparation of Oxygen: Practical experience with methods for generating oxygen gas, such as the catalytic decomposition of hydrogen peroxide.
- Dissolved Oxygen (DO) Measurement: Learning techniques to measure the amount of oxygen dissolved in water or other liquids, which is crucial for environmental monitoring and aquatic life.
- Winkler Method: A classic titration-based chemical method for precisely measuring dissolved oxygen (see a visual example of the setup).
- DO Meters/Probes: Using electronic meters with probes (e.g., electrochemical or optical sensors) for faster, real-time dissolved oxygen measurements in the field (see a visual example of a device).
- Applications in Industry: Discussing the use of oxygen sensors in industrial settings for combustion control, ensuring inert atmospheres, and monitoring gas purity.
Location and Schedule for Best Paramedical Training Center In Bangladesh
Practical classes are held at the HRTD Medical Institute in Mirpur-10, Dhaka. Flexible schedules are available for working professionals, with morning and evening shifts on Fridays, Mondays, and Saturdays. Practicle Class For 6 Month Best Pharmacy Course in Bangladesh
Practical classes at HRTD Medical Institute focus on hands-on instrumental and clinical skills required for working in pharmacies and basic healthcare settings.
Core Practical Skills Covered
The institute offers specific instrumental training as part of its pharmacy courses, which includes:
- Vital Signs Measurement: Learning to measure blood pressure, heart rate, and pulse.
- Respiratory Care: Practical instruction on using inhalers, rotahalers, and nebulizers, as well as saturated oxygen measurement.
- Injectables and Infusions: Training for Intramuscular (IM), Intravenous (IV), and Subcutaneous (SC) injections, along with saline infusion and cannula insertion.
- Dispensing Skills: Training in correctly filling prescriptions, drug handling, and providing healthcare advice.
- First Aid: Basic and intermediate life-saving skills, including CPR, managing bleeding, burns, and fractures.
Course Structures
Practical training is integrated into several pharmacy programs:
- 6-Month Courses: Often referred to as “C Grade Pharmacist” or “Pharmacy Technician” courses, these focus heavily on foundational practical work and preparation for the Pharmacy Council of Bangladesh exam.
Location and Schedule
Practical classes are held at the HRTD Medical Institute in Mirpur-10, Dhaka. Flexible schedules are available for working professionals, with morning and evening shifts on Fridays, Mondays, and Saturdays.
How can I get pharmacy certificate in Bangladesh?
Getting a pharmacy certificate in Bangladesh is not an easy process, but it is possible. In order to become a certified pharmacist in Bangladesh, one must first complete a four-year bachelor’s degree in pharmacy from an accredited university. After completing the degree, the student must then pass a two-part national pharmacy examination. If you want to complete our Pharmacy Courses from HRTD Medical Institute please, contact with us.
After successfully passing the pharmacy examination, the student must then complete a two-year internship program. During the internship, the student will be trained in various aspects of pharmacy practice, including dispensing, compounding, and counseling. After completing the internship, the student must then pass the Bangladesh Pharmacy Council’s final examination. If you want to complete our Pharmacy Courses from HRTD Medical Institute please, contact with us.
After successfully passing the examination, the student will receive a certificate of pharmacy. This certificate is valid for three years and must be renewed on a yearly basis. Upon renewal, the student must complete a number of continuing education courses in order to maintain their certification.
In addition to completing their degree, internship, and examination requirements, the student must also have a valid license from the Bangladesh Pharmacy Council. This license must be renewed on a yearly basis and is issued only after successful completion of the national pharmacy examination.
Once the student has successfully completed all of the necessary requirements for becoming a certified pharmacist in Bangladesh, they can then apply for a job in the field. Pharmacists can work in hospitals, pharmacies, pharmaceutical companies, or even in research facilities.
In conclusion, becoming a certified pharmacist in Bangladesh is not an easy process. However, it is possible and with hard work and dedication, it can be done. Once the student has completed their degree, internship, and examination requirements and obtained a valid license from the Bangladesh Pharmacy Council, they can the
 HRTD Medical Institute
HRTD Medical Institute






One comment
Pingback: প্রাথমিক চিকিৎসকের কোর্স কেন করবেন? মোবাইল 01987-073965