LMAF Training Course Details:
LMAF Training Course 6 Months:
LMAF Training Course 6 Months: Mobile Number 01987-073965, 01797-522136. The shortest LMAF Course is the 6-month LMAF Course. This course contains 5 subjects. The subjects are Human Anatomy & Physiology, Pharmacology-1, First Aid & Treatment, Study of OTC Drugs, and Hematology & Pathology. This shortest LMAF Course is for the primary treatment of rural patients in Bangladesh. Total course fee: Tk 26,500.

LMAF Course 1 Year:
LMAF Course 1 Year: Mobile Number 01987-073965, 01797-522136. The short LMAF Training Course is 1 Year LMAF Course. This course contains 10 subjects. The subjects are Human Anatomy & Physiology, Pharmacology-1, First Aid & Treatment, Study of OTC Drugs, and Hematology & Pathology. This short LMAF Course is for the primary treatment of rural patients in Bangladesh. Total course fee Tk 52500, including admission fee, monthly fee, and exam fee.
Teachers for LMAF Course 2 Years
- Dr. Md. Sakulur Rahman, MBBS, CCD (BIRDEM), Course Director
- Dr. Sanjana Binte Ahmed, BDS, MPH, Assistant Course Director
- Dr. Tisha, MBBS, PGT Gyne, Assistant Course Director
- Dr. Suhana, MBBS, PGT Medicine
- Dr. Danial Hoque, MBBS, C-Card
- Dr. Tisha, MBBS
- Dr. Afrin Jahan, MBBS, PGT Medicine
- Dr. Ananna, MBBS
- Dr. Lamia Afroze, MBBS
- Dr. Amena Afroze Anu, MBBS, PGT Gyne, Assistant Course Director
- Dr. Farhana Antara, MBBS,
- Dr. Nazmun Nahar Juthi, BDS, PGT
- Dr. Farhana Sharna, MBBS
- Dr. Bushra, MBBS
- Dr. Turzo, MBBS
- Dr. Kamrunnahar Keya, BDS, PGT (Dhaka Dental College)
- Dr. Shamima, MBBS, PGT Gyne
- Dr. Alamin, MBBS
- Dr. Benzir Belal, MBBS
- Dr. Disha, MBBS
- Dr. Mahinul Islam, MBBS
- Dr. Tisha, MBBS, PGT Medicine
- Dr. Anika, MBBS, PGT
- Dr. Jannatul Ferdous, MBBS, PGT Gyne
- Dr. Jannatul Aman, MBBS, PGT
- Dr. Rayhan, BPT
- Dr. Abu Hurayra, BPT
- Dr. Sharmin Ankhi, MBBS, PGT Medicine
- Md. Monir Hossain, B Pharm, M Pharm
- Md. Monirul Islam, B Pharm, M Pharm
- Md. Feroj Ahmed, BSc Pathology, PDT Medicine
Some Subjects for the LMAF Training Course in Bangladesh
LMAF Course 2 Years subjects. Mobile No. 01987073965, 01797522136.
- Human Anatomy & Physiology-1
- Pharmacology-1
- Study of OTC Drugs
- First Aid-1 & 2
- Practice of Medicine
- Hematology
- Pathology for Medical Practice
- Cardiovascular Anatomy
- Antimicrobial drugs
- Medical Diagnosis-1 & 2
- Chemistry
- Medical Biochemistry
- Orthopedic Anatomy
- Neuro Anatomy & Physiology
- Human Microbiology
- Surgery.
- Gastro Anatomy & Physiology
- Geriatric Disease & Treatment
Practical Classes for LMAF Training Courses
Heartbeat, Heart Rate, Cardiac Auscultation, Process of Cardiac Auscultation, Tachycardia, Bradycardia, Pulse, Pulse Rate, Strong Pulse, Weak Pulse, Blood Pressure, Normal Blood Pressure, Systolic Blood Pressure, Diastolic Blood Pressure, Pulse Pressure, Mean Blood Pressure, Hypertension, Hypotension, Hypertension Emergency, First Aid and Management of Hypertension Emergency, Cleaning, Dressing, Bandaging, Stitching, Inhaler, Rotahaler, Nebulizer, Pulse Oxymter, Oxygen Cyllinder, Injection Pushing, IM Injection Pushing, IV Injection Pushing, SC Injection Pushing, Vaccine Pushing, Insulin Pushing, Blood Glucose Masurement, Diabetes, Saline Pushing, Respiratory Meter, First Aid and Management of Shock, First Aid of Bone Fracture, X Ray Report Understanding, Respiration, Respiratory Auscultation, Process of Respiratory Auscultation, First Aid of Diarrhea and Constipation, Dehydration Test, Edema Test, Joundice Test, Anemia Test, etc.
Human Anatomy & Physiology For LMAF Training Course in Bangladesh
Important topics in Human Anatomy & Physiology include the study of body systems (like the skeletal, muscular, circulatory, respiratory, digestive, urinary, endocrine, nervous, integumentary, and reproductive systems) and their functions. Specific areas to focus on include the structure and function of cells and tissues, homeostasis, and the principles of anatomy and physiology. Understanding the relationship between structure and function is crucial in this field.
Specific Systems:
- Skeletal System: Bones, cartilage, and joints; their roles in support, protection, and movement.
- Muscular System: Muscles and their functions in movement.
- Circulatory System: The heart, blood vessels, and blood; responsible for transporting oxygen, nutrients, and hormones.
- Respiratory System: Lungs and airways; facilitates gas exchange.
- Digestive System: Mouth, stomach, intestines, etc.; breaks down food and absorbs nutrients.
- Urinary System: Kidneys, bladder, etc.; removes waste from the blood and regulates fluid balance.
- Endocrine System: Glands that produce hormones; regulates various bodily functions.
- Nervous System: Brain, spinal cord, nerves; controls and coordinates body functions.
- Integumentary System: Skin, hair, nails; provides a protective barrier.
- Reproductive System: Organs involved in reproduction.
Pharmacology For LMAF Training Course in Bangladesh
Important topics in Pharmacology include: pharmacokinetics and pharmacodynamics, autonomic nervous system, drugs affecting the cardiovascular system, anti-infectives, and chemotherapy. Other key areas include general pharmacology (drug absorption, distribution, metabolism, excretion, drug interactions, and adverse drug reactions), and specific drug classes like those used in the treatment of autonomic nervous system disorders, respiratory, endocrine, and gastrointestinal conditions.
General Pharmacology:
Pharmacokinetics:
This encompasses the study of how drugs move through the body (absorption, distribution, metabolism, and excretion). Important aspects include bioavailability, first-pass metabolism, plasma protein binding, and factors affecting drug distribution. Understanding first-order and zero-order kinetics is also crucial.
Pharmacodynamics:
This focuses on how drugs interact with the body at a cellular and molecular level, including drug-receptor interactions, dose-response relationships, and mechanisms of drug action. Key concepts include receptor types (e.g., G protein-coupled receptors), drug antagonism (competitive and non-competitive), and drug resistance.
Adverse Drug Reactions (ADRs):
Understanding the types of ADRs, their mechanisms, and how to manage them is essential.
Drug Interactions:
Knowing how drugs can interact with each other (e.g., through enzyme induction or inhibition) and affect their efficacy and toxicity is vital.
Pharmacogenetics/Pharmacogenomics:
This field explores how genetic variations influence drug response.
Specific Systems and Disease States:
- Autonomic Nervous System (ANS): A comprehensive understanding of the ANS is crucial, including cholinergic and adrenergic drugs, anticholinergic agents, and their clinical uses. This includes specific drugs like those used in glaucoma, myasthenia gravis, and motion sickness.
- Cardiovascular System: Important topics include antihypertensive drugs, drugs for angina and myocardial infarction, antiarrhythmics, and drugs used in heart failure.
- Anti-infectives: Focus on antibacterial, antiviral, antifungal, and antiparasitic drugs, including chemotherapy for tuberculosis, leprosy, and malaria.
- Chemotherapy: Understanding the mechanisms of action and resistance to chemotherapeutic agents used in cancer treatment is important.
- Respiratory System: Includes drugs for asthma, COPD, and other respiratory conditions.
- Endocrine System: Important topics include diabetes (oral hypoglycemic agents, insulin), thyroid disorders, and hormonal contraceptives.
- Gastrointestinal System: Drugs used in peptic ulcer disease, GERD, and for managing diarrhea and constipation.
- Musculoskeletal System: Includes drugs for arthritis (NSAIDs, DMARDs), gout, and osteoporosis.
- CNS: Includes drugs for epilepsy, Parkinson’s disease, anxiety, depression, and psychosis.
- Local Anesthetics and Skeletal Muscle Relaxants: Understanding their mechanisms, uses, and adverse effects.
Study of OTC Drugs For LMAF Training Course in Bangladesh
Studying over-the-counter (OTC) drugs is important due to their widespread use, potential for misuse, and the need for responsible self-care practices. Key areas of focus include understanding drug interactions, recognizing potential side effects, and ensuring proper dosage and administration, especially for vulnerable populations.
Here’s a breakdown of important topics:
1. Responsible Use and Self-Medication:
Understanding OTC medications:
Knowing the difference between OTC and prescription drugs, and understanding that OTCs are not completely risk-free, is crucial.
Self-diagnosis:
Consumers need to be aware of when self-treating with OTCs is appropriate and when to seek professional medical advice.
Proper dosage and administration:
Clear labeling, understanding dosage instructions, and recognizing potential interactions with other medications or conditions are essential.
Practice of Medicine For LMAF Training Course in Bangladesh
Important topics in the practice of medicine include clinical skills, medical ethics, patient safety, mental and behavioral health, and palliative care. Additionally, clinical research, medical education, and the care of older patients are crucial aspects of modern medical practice. Understanding common conditions like diabetes mellitus, hypertension, and HIV is also essential.
Core Clinical Areas:
Clinical Skills: This encompasses a broad range of abilities, including physical examination techniques, diagnostic reasoning, and the ability to interpret medical imaging and lab results.
Hospital Medicine: Covers the management of patients within a hospital setting, including acute and chronic disease management, perioperative care, and interdisciplinary collaboration.
Infectious Diseases: Understanding the pathogenesis, diagnosis, and management of various infectious diseases, including bacterial, viral, fungal, and parasitic infections, is critical.
Cardiology: Focuses on the diagnosis and treatment of heart conditions, including coronary artery disease, heart failure, and arrhythmias.
Endocrinology: Deals with hormonal disorders, including diabetes, thyroid disease, and adrenal insufficiency.
Neurology: Involves the study and treatment of neurological disorders, such as stroke, epilepsy, and Parkinson’s disease.
Gastroenterology: Covers disorders of the digestive system, including inflammatory bowel disease, liver disease, and gastrointestinal cancers.
Respiratory Medicine: Focuses on lung diseases, such as asthma, chronic obstructive pulmonary disease (COPD), and pneumonia.
Nephrology: Deals with kidney disease and its management, including dialysis and transplantation.
Rheumatology: Involves the diagnosis and treatment of rheumatic diseases, such as rheumatoid arthritis and lupus.
Hematology: Covers blood disorders, including anemia, leukemia, and lymphoma.
Essential Supporting Disciplines:
- Medical Ethics: Addresses ethical dilemmas that arise in healthcare, such as end-of-life care, informed consent, and confidentiality.
- Patient Safety: Focuses on preventing medical errors and improving the safety of patient care.
- Mental and Behavioral Health: Covers the diagnosis and treatment of mental health conditions, such as depression, anxiety, and schizophrenia.
- Palliative Care: Provides comfort and support to patients with serious illnesses, focusing on pain and symptom management and improving quality of life.
- Geriatrics: Specializes in the care of older adults, addressing age-related health issues and functional decline.
- Medical Education: Involves the training and education of future healthcare professionals.
- Clinical Research: Focuses on the development of new medical knowledge through scientific investigation.
- Genomic Medicine: Involves the use of genetic information to understand, diagnose, and treat diseases.
- Substance Abuse and Addiction: Addresses the diagnosis and treatment of substance use disorders.
- Community Medicine: Focuses on public health and the prevention of disease in communities.
Key Topics in Community Medicine:
- Epidemiology: The study of the distribution and determinants of health-related states or events in specified populations, and the application of this study to the control of health problems.
- Health Promotion and Disease Prevention: Focuses on strategies to promote healthy lifestyles and prevent disease.
- Health Policy and Management: Involves the development and implementation of health policies and programs.
- Environmental Health: Deals with the impact of environmental factors on human health.
- Occupational Health: Focuses on the health of workers in various occupations.
- Nutrition: Deals with the role of food and diet in maintaining health and preventing disease.
Other Important Areas:
- Medical Informatics: Focuses on the use of information technology in healthcare.
Hematology For LMAF Training Course in Bangladesh
Hematology is the branch of medicine focused on blood and blood-forming organs, encompassing the study of blood and its components, as well as blood-related diseases. Key topics include the anatomy of blood (red and white blood cells, platelets, plasma), hemoglobinopathies, hematologic malignancies (like leukemia and lymphoma), anemia, and coagulopathy. It also involves understanding the functions of bone marrow, spleen, and lymph nodes, as well as the processes of hemostasis and thrombosis.
Here’s a more detailed breakdown:
1. Blood and its Components:
Bone Marrow: The site of blood cell production.
Red Blood Cells (Erythrocytes): Carry oxygen from the lungs to the body’s tissues.
White Blood Cells (Leukocytes): Part of the immune system, fighting infection.
Platelets: Involved in blood clotting.
Plasma: The liquid component of blood, containing proteins, electrolytes, and other substances.
Hemoglobin: The protein in red blood cells that carries oxygen.
2. Blood Disorders:
- Anemia: A condition characterized by a deficiency in red blood cells or hemoglobin.
- Hemoglobinopathies: Abnormalities in the structure or production of hemoglobin, such as sickle cell disease.
- Hematologic Malignancies: Cancers of the blood and bone marrow, including leukemia and lymphoma.
- Coagulopathy: Disorders affecting blood clotting, such as hemophilia.
- Thrombocytopenia: Low platelet count, leading to bleeding problems.
- Disorders of Iron Metabolism: Conditions related to iron deficiency or excess.
3. Other Important Areas:
- Hemostasis and Thrombosis: The processes of blood clotting and the formation of blood clots, respectively.
- Transfusion Medicine: The study and practice of blood transfusions.
- Hematologic Oncology: The branch that deals with blood cancers, often in collaboration with oncologists.
- Hematopathology: The study of blood and bone marrow diseases, often performed by hematopathologists.
- Stem Cell Transplantation: A treatment for some hematologic diseases, involving the transplantation of healthy stem cells.
Pathology for Medical Practice For LMAF Training Course in Bangladesh
Pathology, in the context of medical practice, primarily focuses on understanding the causes, mechanisms, and effects of diseases, with a strong emphasis on the structural and functional changes within the body. It involves studying disease at various levels, including molecular, cellular, tissue, and organ levels. The main topics in pathology for medical practice can be broadly categorized into General Pathology, Anatomical Pathology, and Clinical Pathology.
General Pathology: This area covers fundamental concepts about disease, including:
- Etiology: The cause of disease.
- Pathogenesis: The mechanisms of disease development.
- Morphologic Changes: Structural alterations in cells and tissues.
- Clinical Manifestations: The functional consequences of these changes
Anatomical Pathology: This branch focuses on the gross and microscopic examination of tissues and organs, often involving:
- Surgical Pathology: Examination of tissues removed during surgery.
- Cytopathology: Examination of individual cells.
- Autopsy Pathology: Examination of the body after death.
- Forensic Pathology: Investigation of death for legal purposes.
Clinical Pathology: This area involves the analysis of body fluids (like blood and urine) and the application of laboratory techniques to diagnose and monitor diseases. It includes:
- Clinical Chemistry: Analysis of chemical components in body fluids.
- Hematology: Study of blood and blood-forming tissues.
- Microbiology: Identification and characterization of microorganisms.
- Immunology: Study of the immune system and its role in disease.
- Molecular Pathology: Focuses on genetic testing and biomarkers.
Other important topics within pathology include:
- Inflammation and Tissue Repair: Understanding the body’s response to injury.
- Infectious Diseases: Studying diseases caused by pathogens.
- Neoplasia (Cancer): Understanding the development, characteristics, and treatment of tumors.
- Genetic Diseases: Studying diseases caused by inherited or acquired genetic mutations.
- Environmental and Occupational Diseases: Studying diseases related to environmental or workplace exposures.
- Nutritional Disorders: Studying diseases related to nutritional deficiencies or excesses.
- Age-Related Diseases: Studying diseases that are more common in older individuals.
Cardiovascular Anatomy For LMAF Training Course in Bangladesh
Important topics in cardiovascular anatomy include the heart’s structure (chambers, valves, layers, and great vessels), blood vessels (arteries, veins, capillaries), and the circulatory system (pulmonary and systemic circulation). Understanding the heart’s conduction system, cardiac cycle, and blood flow pathways is also crucial.
Detailed Breakdown:
1. The Heart:
- Chambers: Right atrium, left atrium, right ventricle, and left ventricle.
- Valves: Tricuspid, bicuspid (mitral), pulmonary, and aortic valves, ensuring unidirectional blood flow.
- Layers: Endocardium (inner), myocardium (muscle), and pericardium (outer protective layer).
- Great Vessels: Aorta, pulmonary artery, superior and inferior vena cava.
- Conduction System: Sinoatrial (SA) node, atrioventricular (AV) node, bundle of His, bundle branches, and Purkinje fibers, responsible for electrical impulses that regulate heartbeats.
2. Blood Vessels:
- Arteries: Carry oxygenated blood away from the heart (except for the pulmonary artery).
- Veins: Carry deoxygenated blood back to the heart (except for the pulmonary veins).
- Capillaries: Tiny vessels facilitating the exchange of nutrients and waste between blood and tissues.
3. Circulatory System:
- Pulmonary Circulation: The flow of blood between the heart and lungs for oxygenation.
- Systemic Circulation: The flow of blood from the heart to the rest of the body and back.
4. Other Important Aspects:
- Cardiac Cycle: The sequence of events during one heartbeat, including atrial and ventricular contractions and relaxations.
- Blood Pressure: The force exerted by blood against the walls of blood vessels, regulated by factors like baroreceptors and the renin-angiotensin-aldosterone system.
- Coronary Circulation: The blood supply to the heart muscle itself.
- Age-related changes: Physiological changes in the cardiovascular system with age.
Neuro Anatomy for LMAF Training Course in Bangladesh
Main neuroanatomy topics include the central and peripheral nervous systems, the brain’s subdivisions (cerebrum, cerebellum, brainstem), cranial nerves, spinal cord, and protective structures like the meninges and cerebrospinal fluid. Other important areas are the blood supply to the brain and spinal cord, neurodevelopment, and the microscopic structure of neural tissues like white and gray matter.
Major anatomical divisions
- Central Nervous System (CNS): Composed of the brain and spinal cord.
- Brain: Divided into the cerebral hemispheres, cerebellum, and brainstem (medulla, pons, midbrain).
- Spinal Cord: Connects the brain to the peripheral nervous system.
- Peripheral Nervous System (PNS): Includes all nerves outside the brain and spinal cord.
- Cranial Nerves: The 12 pairs of nerves originating from the brainstem, each with a specific function (e.g., optic, facial, vagus).
- Spinal Nerves: Nerves that branch out from the spinal cord.
Protective and supporting structures
- Meninges: The membranes that protect the brain and spinal cord, consisting of the dura mater, arachnoid mater, and pia mater.
- Cerebrospinal Fluid (CSF): A clear fluid that cushions and protects the CNS and is produced within the ventricles.
- Skull and Vertebrae: The bony structures that provide a physical protective layer for the brain and spinal cord.
- Blood-Brain Barrier: A protective layer that prevents harmful substances in the blood from reaching the brain.
Key structures and tracts
- Cerebral Hemispheres: The largest part of the brain, divided into lobes (frontal, parietal, temporal, occipital, and insula) with distinct functions related to motor control, sensation, vision, and hearing.
- Internal Capsule: A major white matter structure that contains ascending and descending tracts.
- Corpus Callosum: A large bundle of nerve fibers connecting the two cerebral hemispheres.
- Gray and White Matter: Gray matter consists of neuronal cell bodies, while white matter consists of myelinated axons that form important tracts.
Circulation and functional areas
- Arterial and Venous Supply: The network of arteries and veins that supply blood to the brain and spinal cord.
- Ascending and Descending Tracts: Nerve pathways in the spinal cord that transmit sensory information up to the brain and motor commands down from the brain.
- Functional Areas: The specific regions of the cerebral cortex responsible for different tasks, such as the primary auditory cortex in the temporal lobe or the visual cortex in the occipital lobe.
Orthopedic Anatomy for LMAF Training Course in Bangladesh
Orthopedic anatomy focuses on the musculoskeletal system and its related structures. The main topics include the detailed anatomy of specific body regions, the components of the musculoskeletal system, and clinically relevant areas such as trauma and pathology.
Regional Anatomy
Orthopedic practice requires a deep understanding of the anatomy of surgically important regions, with a strong focus on the limbs and spine.
- Upper Limb: The shoulder, arm, elbow, forearm, wrist, and hand. Key areas of study include the brachial plexus, rotator cuff muscles, carpal tunnel, and specific fracture types (e.g., Colles’, Supracondylar).
- Lower Limb: The hip, thigh, knee, leg, ankle, and foot. Important topics include the hip and knee joints (and their replacements), cruciate ligaments, meniscal injuries, and various fractures (e.g., femoral neck, tibial plateau).
- Spine: The cervical, thoracic, and lumbar spine. This includes the anatomy of the vertebral column and spinal cord, disc prolapse, scoliosis, and conditions like cauda equina syndrome.
Components of the Musculoskeletal System
The foundational knowledge covers all the interconnected parts of the system:
- Bones (Osteology): Structure, function, growth plates, and different types of bones (compact and cancellous).
- Joints: Types of joints, their function, movement (flexion, extension, rotation, etc.), ligaments, and cartilage.
- Muscles: Origin, insertion, nerve supply, and function of key muscles and muscle groups (e.g., rotator cuff).
- Nerves (Neuroanatomy): Major peripheral nerves (e.g., sciatic, median, ulnar, radial) including their course, relations, and the clinical implications of nerve injuries.
- Vasculature: The major arteries and veins supplying different regions, and their surgical significance.
Clinically Relevant Topics
Anatomy is applied to the diagnosis and treatment of a wide range of conditions:
- Trauma: General principles of fracture and dislocation management, open fractures, compartment syndrome, and specific injuries in adults and pediatrics.
- Pathology and Diseases: Bone infections (osteomyelitis, septic arthritis), tumors (benign and malignant), metabolic bone diseases (osteoporosis, rickets), and arthritic conditions (osteoarthritis, rheumatoid arthritis).
- Pediatrics: Congenital disorders (clubfoot, developmental dysplasia of the hip) and growth-related conditions (Slipped Capital Femoral Epiphysis).
- Surgical Approaches: The anatomical knowledge necessary for surgical procedures, including surface anatomy and the location of nerves and vessels during approaches.
Human Microbiology for LMAF Training Course in Bangladesh
The main topics in human microbiology cover the biology of various microorganisms (bacteria, viruses, fungi, and parasites) and their interactions with the human host, with a strong emphasis on disease, immunity, and control.
Core subjects typically include:
- Introduction to Microbiology: History of the field, the germ theory of disease, microscopy, and fundamental differences in the structure and function of prokaryotic and eukaryotic cells, as well as the basic characteristics of viruses.
- Medical Microbiology: The study of microorganisms that cause diseases in humans (pathogens). This covers their identification, modes of transmission, mechanisms of infection (pathogenesis), and the clinical manifestations of the diseases they cause.
- Immunology: The study of the host’s immune system and its response to infectious agents. Topics include innate and adaptive immunity, the components of the immune system (cells, organs, antibodies), immune disorders (autoimmunity, immunodeficiency), and the principles of vaccination.
- Bacteriology: A detailed focus on bacteria, including their classification, genetics, metabolism, growth, and methods for control (antibiotics and resistance mechanisms).
- Virology: The study of viruses, their structure, replication cycles, and pathogenesis, as well as specific details on major human viruses like HIV, Hepatitis B, and influenza.
- Mycology & Parasitology: Coverage of pathogenic fungi, protozoa, and helminths (worms), the diseases they cause (e.g., malaria), and their complex life cycles and interactions with the host.
- Microbial Genetics & Molecular Biology: The mechanisms of genetic information flow in microorganisms, including DNA replication, gene expression, mutations, gene transfer (conjugation, transduction, transformation), and the principles of genetic engineering.
- Clinical & Diagnostic Microbiology: Practical laboratory techniques for the isolation, cultivation, staining, and identification of pathogenic microorganisms from clinical specimens. This also involves antimicrobial susceptibility testing and the use of modern molecular diagnostic methods.
- Epidemiology and Public Health: The study of how infections spread within populations and the strategies used for their prevention and control, including infection control practices.
- Human Microbiome: The role of the normal resident microflora of the human body and how these communities influence health and disease.
These topics often integrate with other fields like biochemistry, cell biology, and pharmacology to provide a comprehensive understanding of microorganisms and their impact on human health.
Medical Biochemistry for LMAF Training Course in Bangladesh
Main topics in medical biochemistry include carbohydrate, lipid, and protein metabolism; enzymes and bioenergetics; and the molecular biology of the cell and its processes. Other key areas are cell and molecular biology, genetics, endocrinology, and the biochemistry of human diseases and nutrition.
Metabolic pathways
- Carbohydrate metabolism: Glycolysis, gluconeogenesis, the TCA cycle, and disorders like diabetes.
- Lipid metabolism: Fatty acid synthesis and breakdown, cholesterol metabolism, and lipoproteins (HDL, LDL, VLDL).
- Protein and amino acid metabolism: Amino acid catabolism, the urea cycle, and protein structure and synthesis.
- Bioenergetics: Biological oxidation, the respiratory chain, oxidative phosphorylation, and ATP production.
Molecular and cellular biochemistry
- Molecular biology: DNA replication, transcription, translation, and gene expression.
- Cell biology: Cell structure, membrane permeability, and intracellular communication.
- Enzymology: Enzyme classification, kinetics, regulation, and factors affecting enzyme activity.
- Genetics and genetic diseases: Molecular basis of inherited diseases and genetic code.
Clinical and specialized topics
- Endocrinology: The role of hormones, including their synthesis and mechanism of action.
- Nutrition: The role of vitamins, minerals, and other nutrients in metabolic processes.
- Pathology: The biochemical basis of diseases, such as cancer and metabolic disorders.
- Immunology: The biochemistry of the immune system.
Other relevant subjects
- Organic Chemistry: Provides the foundational chemical principles, including stereochemistry and reaction mechanisms.
- Statistics and Bioinformatics: Used for analyzing experimental data and biological information.
Surgery for LMAF Training Course in Bangladesh
Main topics in surgery can be broadly categorized by organ systems (e.g., cardiovascular, gastrointestinal, musculoskeletal) and surgical specialties (e.g., general surgery, neurosurgery, trauma surgery). Other core subjects include foundational sciences (anatomy, physiology), pre-operative and post-operative care (anesthesia, wound healing, resuscitation), and patient-focused areas like patient safety and medical ethics.
By organ system
- Gastrointestinal: The most heavily weighted system in some exams, covering conditions of the stomach, intestines, liver, and gallbladder.
- Cardiovascular: Includes heart and blood vessel diseases and their surgical management.
- Respiratory: Deals with surgical issues of the lungs and airways.
- Musculoskeletal: Covers bone and muscle injuries, joints, and related conditions.
- Genitourinary: Includes both the renal/urinary system and the female and male reproductive systems.
- Endocrine: Focuses on surgical problems of glands and hormones.
- Breast and Lymphoreticular: Includes the surgical aspects of breast diseases and the blood and lymph systems.
- Neurological: Surgical issues of the brain, spinal cord, and nerves.
By surgical specialty
- General Surgery: The foundational discipline covering a broad range of common surgical problems.
- Trauma Surgery: Manages surgical care for victims of traumatic injuries.
- Pediatric Surgery: Focuses on surgical conditions in children.
- Cardiothoracic Surgery: Operates on the heart and lungs.
- Vascular Surgery: Specializes in the arteries and veins.
- Oncology: Deals with the surgical treatment of cancer.
- Plastic and Reconstructive Surgery: Includes cosmetic and reconstructive procedures.
- Orthopedic Surgery: Deals with the musculoskeletal system.
- Ophthalmology: Surgery of the eye.
- Otolaryngology (ENT): Surgery of the Ear, Nose, and Throat.
Foundational and cross-cutting topics
- Anesthesia and Perioperative Care: Includes anesthetic methods, pre-operative assessment, and post-operative management.
- Wound Healing: The biological process, factors influencing it, and management of different types of wounds.
- Shock and Resuscitation: The causes, types, and management of shock, including life support.
- Medical Ethics and Jurisprudence: Legal and ethical issues related to surgical practice.
- Patient Safety: Practices to prevent harm to patients.
- Pain Management: Strategies for managing surgical pain.
Medical Diagnosis 1 & 2 for LMAF Training Course in Bangladesh
The main topics of study for medical diagnosis encompass foundational sciences, clinical disciplines, and specific information-gathering activities. These areas provide the necessary knowledge and skills for healthcare professionals to identify diseases accurately.
Foundational Sciences
These subjects form the essential basis for understanding the human body and disease processes.
- Anatomy: The study of the structure of the body, which is crucial for the physical examination and interpreting imaging studies.
- Physiology: The study of normal bodily functions. Understanding normal function is essential to recognize deviations caused by disease (pathophysiology).
- Biochemistry: Focuses on the chemical processes within living organisms, helping to understand metabolic disorders and analyze lab results.
- Pathology: The study of the causes and effects of disease or injury, which is central to understanding how diseases progress.
- Microbiology: The study of microorganisms, including bacteria, viruses, and fungi, which is vital for diagnosing infectious diseases.
- Genetics: The study of heredity and gene function, critical for diagnosing genetic disorders and understanding individual health risks.
- Pharmacology: The study of drugs and their effects, necessary for understanding how treatments interact with diseases.
Clinical Disciplines
These areas apply foundational knowledge in a clinical setting to diagnose specific conditions.
- Internal Medicine: A broad field covering the diagnosis and non-surgical treatment of diseases in adults.
- Radiology (Diagnostic Imaging): The use of imaging modalities like X-rays, CT scans, MRI, and ultrasound to diagnose diseases and injuries.
- Laboratory Medicine: Includes various sub-disciplines that use laboratory tests to analyze patient samples (blood, urine, tissue).
- Clinical Chemistry: Analyzes chemical components in bodily fluids.
- Hematology: Focuses on the diagnosis of blood-related disorders, such as anemia or leukemia.
- Immunology: Deals with the immune system and related diseases or disorders.
- Clinical Skills: Covers the practical application of knowledge, including patient history taking, physical examinations, and patient interviews.
Core Components of the Diagnostic Process
The process of medical diagnosis itself involves specific activities and areas of consideration.
- Clinical History and Interview: Gathering information about a patient’s symptoms, medical history, and lifestyle.
- Physical Examination: A systematic assessment of the patient’s body for signs of illness.
- Diagnostic Testing: Ordering and interpreting various tests, including lab work and imaging studies.
- Referrals and Consultations: Involving other specialists when a condition requires specific expertise.
- Diagnostic Reasoning: The cognitive process physicians use to integrate information and formulate a diagnosis, considering factors like probability and diagnostic uncertainty.
Antimicrobial Drug for LMAF Training Course in Bangladesh
The most important topics relating to antimicrobial drugs center on their mechanisms of action, their proper use in medicine (pharmacology), and the global public health crisis of antimicrobial resistance (AMR).
Antimicrobial Resistance (AMR)
AMR is arguably the most critical topic, as it threatens the effectiveness of modern medicine.
- Global Health Threat: AMR is one of the top ten global public health threats, responsible for an estimated 1.27 million deaths in 2019. Drug-resistant infections (sometimes called “superbugs”) make common procedures like surgery and chemotherapy much riskier.
- Main Drivers: The primary causes of AMR are the misuse and overuse of antimicrobials in human health, animal agriculture, and plant cultivation.
- One Health Approach: Addressing AMR requires a coordinated, multi-sectoral strategy (human, animal, and environmental health) known as the “One Health” approach, as resistance genes can pass between these sectors.
- Stewardship: Antimicrobial stewardship, the systematic effort to educate healthcare professionals on evidence-based prescribing, is a key strategy to optimize use and reduce resistance.
Mechanisms of Action
Understanding how these drugs work is fundamental to their study and development. Antimicrobials generally operate by targeting specific functions in the microbe that are different from the host’s cells.
The major modes of action for antibacterials include:
- Inhibition of cell wall synthesis: Beta-lactams (penicillins, cephalosporins) and glycopeptides (vancomycin) work this way.
- Inhibition of protein synthesis: Aminoglycosides, tetracyclines, and macrolides bind to bacterial ribosomes.
- Interference with nucleic acid synthesis: Fluoroquinolones (ciprofloxacin) and rifamycins inhibit DNA gyrase or RNA polymerase.
- Inhibition of a metabolic pathway: Sulfonamides and trimethoprim block the synthesis of folic acid, which is essential for microbial growth.
- Impairment of cell membrane function: Polymyxins disrupt the bacterial cell membrane.
Classification and Pharmacology
Antimicrobial drugs are classified in various ways, which informs clinical practice.
- Spectrum of Activity: Drugs can be broad-spectrum (effective against a wide range of microbes) or narrow-spectrum (effective against specific groups).
- Effect on Microbes: They are either bactericidal (kill bacteria) or bacteriostatic (inhibit their growth, allowing the immune system to clear the infection).
- Types: The term “antimicrobial” is an umbrella term for:
- Antibiotics (antibacterials)
- Antifungals
- Antivirals
- Antiparasitics
- Pharmacokinetics: Important factors include how well a drug penetrates specific tissues (like the blood-brain barrier), its half-life, and how it is eliminated from the body.
New Research and Development
The development of new antimicrobials has slowed, leading to a “pipeline and access crisis”. Research efforts are now focused on novel approaches to combat existing resistance, including the use of nanotechnology, natural products, and phage-based therapies.
Gastro Anatomy for LMAF Training Course in Bangladesh
The most important topics in gastrointestinal (GI) anatomy cover the structure of the entire gastrointestinal tract, the accessory organs that aid digestion, and the histological layers that facilitate the system’s functions.
Key Organs and Structures
The GI system is composed of the alimentary canal (a continuous tube from mouth to anus) and accessory organs.
- Mouth/Oral Cavity: The entry point for ingestion and initial mechanical (chewing) and chemical (salivary amylase for starches, lingual lipase for fats) breakdown.
- Pharynx & Esophagus: Muscular tubes responsible for propelling food from the mouth to the stomach via swallowing and peristalsis, with no significant digestion or absorption occurring here.
- Stomach: A J-shaped muscular organ that stores food, mixes it with strong acids (hydrochloric acid) and enzymes (pepsin for proteins) to form chyme, and has an additional oblique muscle layer for churning.
- Small Intestine: The primary site for chemical digestion and nutrient absorption, a long tube divided into three segments:
- Duodenum: Receives chyme from the stomach and digestive juices (bile and pancreatic enzymes) from accessory organs.
- Jejunum: The main site for nutrient and water absorption.
- Ileum: Primarily absorbs vitamin B12 and bile acids.
- Large Intestine: Responsible for absorbing most of the remaining water and electrolytes, forming and storing feces, and hosting beneficial gut bacteria that produce vitamins like K. It is divided into the cecum, ascending, transverse, descending, and sigmoid colons, and the rectum.
- Rectum & Anus: The rectum stores feces before elimination (defecation) through the anal canal and anus, controlled by internal and external anal sphincters.
Accessory Organs
These organs are crucial for digestion but food does not pass through them directly.
- Salivary Glands: Secrete saliva to moisten food and begin carbohydrate and lipid digestion.
- Liver: The largest internal organ, produces bile which emulsifies fats in the small intestine to aid digestion.
- Gallbladder: Stores and concentrates bile produced by the liver, releasing it into the duodenum when needed.
- Pancreas: Secretes a bicarbonate-rich fluid to neutralize stomach acid and releases crucial digestive enzymes (amylases, lipases, proteases) into the small intestine.
Histological Layers
The entire GI tract, from the esophagus to the anal canal, shares a common basic four-layered structure, with variations reflecting specialized functions in different regions.
- Mucosa: The innermost layer, responsible for most digestive, absorptive, and secretory processes. It features specialized epithelial cells (e.g., villi and microvilli in the small intestine for increased surface area).
- Submucosa: A connective tissue layer containing blood vessels, lymphatics, and nerves (submucosal plexus).
- Muscularis Externa: Composed of an inner circular and outer longitudinal smooth muscle layer (with an additional inner oblique layer in the stomach) that coordinates the movement of food through the tract via peristalsis.
- Serosa/Adventitia: The outermost protective layer; serosa covers intraperitoneal organs, while adventitia covers retroperitoneal organs.
Geriatric Disease & Treatment for LMAF Training Course in Bangladesh
The most important topics in geriatric disease and treatment center on managing multifactorial conditions (geriatric syndromes) and maintaining functional independence. These areas require a specialized, person-centered approach that considers the interplay of multiple chronic conditions, medication management, and overall quality of life.
Core Areas in Geriatric Health
Geriatric care focuses on several key domains, often summarized by the “5 M’s” framework:
- Mind: Addressing cognitive and emotional well-being, including screening and management of dementia, delirium, and depression.
- Mobility: Maintaining physical function and independence through fall prevention, exercise, and addressing musculoskeletal issues like arthritis and osteoporosis.
- Medications: Managing polypharmacy (the use of multiple medications) to avoid adverse drug effects and interactions, often using resources like the AGS Beers Criteria.
- Multicomplexity: Coordinating care for patients with multiple chronic conditions (e.g., heart disease, diabetes, cancer) and understanding how these conditions interact.
- What Matters Most: Prioritizing the patient’s own goals, values, and preferences to guide treatment decisions and ensure person-centered care.
Very Important Topics & Conditions
Key topics within these domains that are particularly important due to their prevalence and impact on quality of life include:
Geriatric Syndromes
These conditions are common in older adults, multifactorial in origin, and often don’t fit into a single disease category.
- Falls and Gait Disorders: A leading cause of serious injury, falls often stem from a combination of factors including vision problems, muscle weakness, and medication side effects.
- Urinary Incontinence: While common, it is not an inevitable part of aging and can often be managed or improved with proper assessment and treatment.
- Frailty: Characterized by decreased physiological reserves and increased vulnerability to stressors, frailty is a key predictor of poor health outcomes and disability.
- Delirium: A sudden state of severe confusion, often triggered by acute illness or injury (like an infection or surgery), that requires immediate medical attention.
Chronic Diseases
Older adults often manage multiple chronic conditions that require ongoing attention.
- Cardiovascular Diseases: Including hypertension, heart failure, and stroke, which are the leading causes of death in older adults.
- Neurocognitive Disorders: Such as Alzheimer’s disease and other forms of dementia, which significantly impact memory, thinking, and daily function.
- Musculoskeletal Disorders: Osteoarthritis, osteoporosis, and sarcopenia (muscle loss) are frequent causes of pain, reduced mobility, and functional decline.
- Diabetes: Management is crucial and complicated by the potential for interaction with geriatric syndromes, such as cognitive decline affecting self-care.
Treatment and Management Principles
Effective treatment in geriatrics emphasizes:
- Comprehensive Geriatric Assessment (CGA): A multidimensional evaluation by an interdisciplinary team (physicians, nurses, physical/occupational therapists, social workers, pharmacists) to create a holistic care plan.
- Person-Centered Care: Tailoring interventions to the individual’s specific priorities and life expectancy.
- Preventive Health: Utilizing appropriate immunizations (flu, pneumonia, shingles, COVID-19) and screenings, and promoting healthy lifestyle measures like diet and exercise to maintain function.
- Palliative and End-of-Life Care: Discussions about advanced care planning and end-of-life preferences are essential components of comprehensive geriatric care, focusing on comfort and dignity.
Practical Class on Heartbeat
A heartbeat is the rhythmic contraction and relaxation of the heart, driven by electrical signals, pumping blood through the body; it involves phases like diastole (relaxation/filling) and systole (contraction/pumping) and is measured as beats per minute (BPM), with 60-100 BPM being a normal resting range for adults, though it varies with activity. The electrical impulse originates at the sinoatrial (SA) node, travels through the atria, and then to the ventricles, causing them to contract and pump oxygenated and deoxygenated blood.
How it works (The Cardiac Cycle)
- Diastole (Relaxation): The heart’s chambers relax, and blood flows from the body into the right atrium and from the lungs into the left atrium, then into the ventricles.
- Atrial Systole: The atria contract, pushing remaining blood into the ventricles.
- Ventricular Systole: The ventricles contract forcefully, pushing blood out: the right side sends it to the lungs, and the left side pumps it to the rest of the body.
- Cycle Repeats: The heart then re-enters diastole, refilling with blood.
Key Terms
- SA Node: The heart’s natural pacemaker, initiating the electrical signal.
- Pulse: The palpable wave of blood flow from the heart’s beat.
- Heart Rate: The number of beats per minute (BPM).
- Tachycardia: A heart rate over 100 BPM at rest.
- Bradycardia: A slow heart rate (not mentioned in snippets, but implied opposite of tachycardia).
What affects it
- Factors Such as Stress, caffeine, nicotine, exercise, and hormones can increase heart rate.
- Normal Range: 60-100 BPM at rest for most adults, though athletes often have lower rates.
Practical Class on Heart Rate
Heart rate is the number of times your heart beats per minute (bpm), with a normal resting rate for adults generally being 60-100 bpm, though it varies with age, fitness, stress, and medications, with athletes often having lower rates. It’s a key health indicator, reflecting heart function; a consistently high rate (tachycardia, >100 bpm at rest) or low rate (bradycardia, <60 bpm at rest, unless fit) can signal issues. You can check it by feeling your pulse at the wrist or with devices, ideally after resting.
Normal Ranges & Factors
- Adults: 60-100 bpm resting.
- Athletes: Can be as low as 40 bpm or less.
- Children: Have higher rates, e.g., 80-120 bpm for ages 3-5.
- Factors Affecting It: Fitness, emotions, caffeine, alcohol, medications, illness, pregnancy, and sleep quality.
How to Check Your Heart Rate
- Rest: Sit quietly for 5-10 minutes.
- Locate Pulse: Place index and middle fingers on the thumb side of your wrist.
- Count: Count beats for 15 seconds and multiply by 4, or count for a full minute.
- Devices: Smartwatches and fitness trackers offer easy monitoring.
Practical Class on Tachycardia
Tachycardia is a heart rhythm disorder where the heart beats too fast, typically over 100 beats per minute (bpm) at rest in adults, signaling an electrical problem or normal response to stress, exercise, or underlying conditions like fever, anemia, anxiety, or thyroid issues, causing symptoms like palpitations, dizziness, and shortness of breath, requiring medical evaluation to determine if it’s benign (sinus tachycardia) or a serious arrhythmia needing treatment.
Types of Tachycardia
- Sinus Tachycardia: A normal response to stress, fever, or exercise, where the sinus node fires too quickly.
- Supraventricular Tachycardia (SVT): Abnormal signals start above the ventricles, causing sudden, rapid heartbeats, often felt as palpitations.
- Ventricular Tachycardia (VT): A dangerous rhythm originating in the heart’s lower chambers, potentially life-threatening.
- Atrial Fibrillation (AFib) & Flutter: Irregular, rapid heartbeats in the upper chambers (atria).
Common Symptoms
Racing heart or palpitations, Dizziness or lightheadedness, Shortness of breath, and Chest pain or discomfort.
Common Causes & Triggers
- Lifestyle: Caffeine, alcohol, stimulants, smoking, stress, lack of sleep.
- Medical Conditions: Fever, anemia, thyroid disease, dehydration, lung disease, sleep apnea, heart disease, and high blood pressure.
- Electrical Issues: Faulty heart wiring or triggers in the heart’s chambers.
Practical Class on Bradycardia
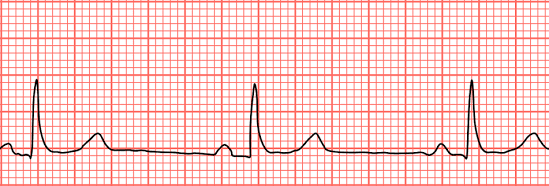

Bradycardia is a slower-than-normal heart rate, typically under 60 beats per minute (bpm) in adults at rest, caused by issues with the heart’s electrical system, certain medications, or underlying conditions like sleep apnea or thyroid problems, leading to symptoms like dizziness, fatigue, shortness of breath, and confusion, though highly fit individuals and athletes may have a normal slow rate. Treatment varies by cause, ranging from lifestyle changes to pacemakers, and involves diagnosing the underlying problem with tools like an EKG.
What it is
- A heart rate below 60 bpm, meaning the heart isn’t pumping enough oxygen-rich blood to the body.
- Can be normal for athletes or during sleep, but problematic if it causes symptoms.
Common types
- Sinus Bradycardia: Slowing of the heart’s natural pacemaker (sinus node).
- Heart Block: Electrical signals from the upper to lower heart chambers are blocked.
Causes
- Heart Issues: Heart disease, previous heart attacks, sick sinus syndrome.
- Medications: Beta-blockers, calcium channel blockers.
- Medical Conditions: Thyroid problems, electrolyte imbalances, sleep apnea, and inflammation.
- Lifestyle: Intense physical fitness (often normal), aging.
Symptoms (when problematic)
- Dizziness, lightheadedness, fainting.
- Fatigue, weakness.
- Shortness of breath, chest pain.
- Confusion or memory problems.
Diagnosis & Treatment
- Diagnosis: Physical exam, EKG, Holter monitor, sleep study, blood tests.
- Treatment: Addressing the cause (e.g., changing meds, treating sleep apnea) or using a pacemaker for severe cases.
Practical Class on IM Injection Pushing
The process of pushing an intramuscular (IM) injection involves a smooth, steady depression of the plunger after the needle is securely in the muscle, ensuring the medication goes in slowly to minimize discomfort, followed by quickly withdrawing the needle at the same angle and activating the safety device, then applying gentle pressure to the site with gauze. Key steps include site preparation (cleaning, Z-track method), swift 90-degree needle insertion, slow plunger push (counting to three), quick withdrawal, and immediate disposal in a sharps container.
Pre-Injection Steps (Preparation)
- Hand Hygiene & Supplies: Wash hands thoroughly and gather medication, syringe, alcohol swabs, gauze, and a sharps container.
- Site Selection & Prep: Locate the correct muscle (e.g., deltoid, ventrogluteal), clean with an alcohol swab, and let it dry.
- Z-Track Method (Optional but Recommended): Use your non-dominant hand to pull the skin and tissue to the side to prevent medication leakage into subcutaneous tissue.
- Syringe Prep: Remove the cap, ensure no large air bubbles, and tap to get a drop of medication at the tip.
The “Push” (Injection)
- Insertion: Hold the syringe like a dart and insert the needle quickly at a 90-degree angle into the muscle.
- Stabilize: Once in the muscle, use your non-dominant hand to steady the syringe.
- Depress Plunger: Slowly and steadily push the plunger all the way down, counting to three.
- Withdrawal: After the fluid is in, hold for a few seconds (around 10 for some meds), then pull the needle straight out at the same 90-degree angle.
Post-Injection Steps
- Safety: Immediately activate the needle’s safety shield and dispose of the entire syringe in the sharps container.
- Site Care: Apply gentle pressure with gauze or a cotton ball (no rubbing) and secure with a bandage if needed.
- Observe: Monitor the patient for any adverse reactions.
Process of IV Injection Pushing
The process of IV Injection Pushing (or Bolus) involves a trained healthcare professional manually injecting medication directly into an established IV line using a syringe, following strict steps: verify order, prepare patient, scrub the IV port (clave), flush with saline to check for patency, attach the medication syringe, push the drug at a specific rate (seconds to minutes) while monitoring, and then perform a post-flush to clear the line, ensuring patient safety and proper delivery.
Key Steps in IV Push Administration
- Preparation & Verification:
- Confirm the doctor’s order, patient details, medication rights (right drug, dose, time, route, patient, documentation, reason, response).
- Gather supplies: saline flush, medication syringe, alcohol wipes, and gloves.
- Perform hand hygiene and don gloves.
- Educate the patient about the medication and potential side effects.
- Priming & Flushing (SASH Method):
- Saline Flush: Scrub the injection port (clave) with an alcohol wipe for 15-30 seconds, let it air dry, then inject 3-5mL of saline to check for patency (blood return) and clear the line.
- Medication Administration:
- Attach Medication: Attach the pre-filled medication syringe (air expelled) to the scrubbed port and twist clockwise to secure.
- Slow Push: Slowly inject the medication at the prescribed rate (e.g., over 1 minute, 2 minutes). Use a timer for accuracy; break down the volume into smaller intervals for easier pacing (e.g., 0.5mL every 30 seconds for a 1mL/min push).
- Completion (SASH):
- HFollow-up Flush: After the medication, flush with another 3-5mL of saline at the same rate as the medication push to ensure all drug enters the bloodstream and clears the tubing, preventing incompatibility with other IV fluids.
- Secure the port with a new alcohol cap if required by facility policy.
Important Considerations
- Timing is Crucial: Pushing too fast can cause adverse effects or medication waste; too slow might delay treatment.
- Compatibility: Always check if the medication is compatible with the primary IV fluid running, if any.
- Patient Monitoring: Closely watch the patient for any adverse reactions during and after administration, especially respiratory changes, notes LevelUpRN.
 HRTD Medical Institute
HRTD Medical Institute






2 comments
Pingback: Diploma in Dental (DID) Course 4 Years Mobile 01987-073965
Pingback: 3 And 6 month pharmacy courses in Dhaka