Nursing Training Course( 1 Year) Course Details:
Nursing Training Course( 1 Year): Mobile No. 01941-123488, 01797-522136. This course contains 10 subjects in 2 semesters. 1st semester contains 5 subjects which are Human Anatomy & Physiology, Chemistry & Pharmacology, First Aid & Treatment, Study of OTC Drugs, and Hematology & Pathology. The 2nd semester contains 5 subjects which are Cardiovascular Nursing, Orthopedic Nursing, General Nursing, Gynecological Nursing, and Clinical Nursing with Practical.

Course Fee Summary:
Course Fee: Admission Fee Tk 10500, Monthly Fee Tk 3000×12=Tk 36000, Exam Fee Tk 3000×2=6000. Total Course Fee Tk 52,500.
Eligibility for Admission: SSC, HSC, Bachelor Degree, Master Degree from Any background.
Job Opportunities:
Private hospitals, Private clinics, Health centers of NGOs, Health centers of Schools and Colleges, Health centers of private companies, Health centers of the Garments Industry, and the Reputed Doctors’ Chamber for pushing injections, saline, and canula and for cleaning, dressing, and bandaging. Job opportunities in Model pharmacy for pushing injections, saline, and canula and for cleaning, dressing, and bandaging. Hospitals in foreign countries.
Location of Nursing Training Course in Dhaka, Bangladesh
Location of Nursing Training Center. Mobile No. 01987-073965, 01797-522136. HRTD Medical Institute, Abdul Ali Madbor Mansion, Section-6, Block-Kha, Road-1, Plot-11, Mirpur-10 Golchattar, Metro Rail Piller No. 249, Dhaka-1216.
Our Others Course:
Pharmacy Course, Dental Course, Nursing Course, Pathology Course, Homeopathy Course, Veterinary Course, Village Doctor Course, PDT( Post Diploma Training) Course, PPT, LMAF Training Course, LMAFP Course, Poultry Course, DMA ( Diploma Medical Assistant), Diploma in Medicine and Surgery (DMDS).
Hostel Facilities in HRTD Medical Institute
Hostal & Meal Facilities
The Institute has hostel facilities for the students. Students can take a bed in the hostel.
Hostel Fee Tk 3000/- Per Month
Meal Charges Tk 3000/- Per Month. ( Approximately )
হোস্টাল ও খাবার সুবিধা
ইনস্টিটিউটে শিক্ষার্থীদের জন্য হোস্টেল সুবিধা রয়েছে। ছাত্ররা হোস্টেলে বিছানা নিতে পারে।
হোস্টেল ফি 3000/- টাকা প্রতি মাসে,
খাবারের চার্জ 3000/- টাকা প্রতি মাসে।(প্রায়)
Address of HRTD Medical Institute
আমাদের ঠিকানাঃ HRTD মেডিকেল ইন্সটিটিউট, আব্দুল আলী মাদবর ম্যানশন, সেকশন ৬, ব্লোক খ, রোড ১, প্লট ১১, মেট্রোরেল পিলার নাম্বার ২৪৯, ফলপট্টি মসজিদ গলি, মিরপুর ১০ গোলচত্ত্বর, ঢাকা ১২১৬ । মোবাইল ফোন নাম্বার ০১৭৯৭৫২২১৩৬, ০১৯৮৭০৭৩৯৬৫ ।
Our Address: HRTD Medical Institute, Abdul Ali Madbor Mansion, Section-6, Block- Kha, Road- 1, Plot- 11, Metro Rail Pilar No. 249, Falpatty Mosjid Goli, Mirpur-10 Golchattar, Dhaka 1216. Mobile Phone No. 01797522136, 01987073965.
Subjects of Nursing Training Course in Dhaka, Bangladesh
Subjects of Nursing Training Course 6m & 1 year in Dhaka, Bangladesh Mobile No. 01987-073965, 01797-522136.
Human Anatomy & Physiology Pharmacology Study Of OTC Drugs, First Aid1 & 2, Hematology & Pathology General Chemistry, Cardiovascular Nursing, Gynecological Nursing, General Nursing, Clinical Nursing, Orthopedic Nursing, Pediatric Nursing, etc.
Teacher For Nursing Training Course(NTC 1 Year)
- Dr. Md. Sakulur Rahman, MBBS, CCD (BIRDEM), Course Director
- Dr. Sanjana Binte Ahmed, BDS, MPH, Assistant Course Director
- Dr. Tisha, MBBS, PGT Gyne, Assistant Course Director
- Dr. Suhana, MBBS, PGT Medicine
- Dr. Danial Hoque, MBBS, C-Card
- Dr. Tisha, MBBS
- Dr. Afrin Jahan, MBBS, PGT Medicine
- Dr. Ananna, MBBS
- Dr. Lamia Afroze, MBBS
- Dr. Amena Afroze Anu, MBBS, PGT Gyne, Assistant Course Director
- Dr. Farhana Antara, MBBS,
- Dr. Nazmun Nahar Juthi, BDS, PGT
- Dr. Farhana Sharna, MBBS
- Dr. Bushra, MBBS
- Dr. Turzo, MBBS
- Dr. Kamrunnahar Keya, BDS, PGT (Dhaka Dental College)
- Dr. Shamima, MBBS, PGT Gyne
- Dr. Alamin, MBBS
- Dr. Benzir Belal, MBBS
- Dr. Disha, MBBS
- Dr. Mahinul Islam, MBBS
- Dr. Tisha, MBBS, PGT Medicine
- Dr. Anika, MBBS
- Dr. Sharmin Sultana, DVM, MS, Assistant Course Director
- Dr. Arefin Habib, DVM, MS, Assistant Course Director
- Dr. Habiba, MBBS, PGT
- Dr. Mosharof Hossain, DVM, MS, Ph D
- Dr. Moniruzzaman, DVM, MS
- Dr. Jannatul Ferdous, MBBS, PGT Gyne
- Dr. Jannatul Aman, MBBS, PGT
- Dr. Rayhan, BPT
- Dr. Abu Hurayra, BPT
- Dr. Sharmin Ankhi, MBBS, PGT Medicine
- Md. Monir Hossain, B Pharm, M Pharm
- Md. Monirul Islam, B Pharm, M Pharm
- Md. Feroj Ahmed, BSc Pathology, PDT Medicine
- Dr. Kazi Fetema, DVM, MS
Total Nursing Course of HRTD Medical Institute
- 6 Months Nursing Course
- 1 Year Nursing Course
- 2 Years Nursing Course
- 3 Years Nursing Course
- 4 Years Nursing Course
Practical Works for Nursing Training Course at HRTD Medical Institute
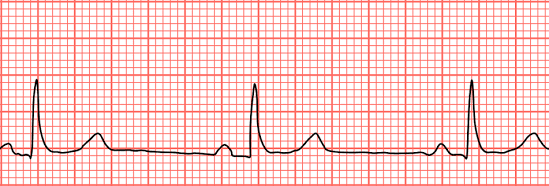
- Heart Beat, Heart Rate
- Heart Sound, Pulse
- Blood Pressure, Hypertension, Hypotension
- First Aid Box
- Auscultation
- Inhaler
- Rota Haler
- Nebulizer
- Glucometer Blood Glucose (Diabetes)
- Injection I/V,I/M
- Cleaning ,Dressing, Bandaging
- Saline
- CPR
- Stitch
- Body Temperature
- Blood Grouping
- Nasal tube Gel, Handwash
Blood Glucose Measurement, Hyperglycemia, Diabetes, Type 1 Diabetes, Type 2 Diabetes, Injection Pushing, IM Injection Pushing, IV Injection Pushing, SC Injection Pushing, ID Injection Pushing, Cannula Setting, the Dosage form of Drugs, Application of medicine through oral route, Application of Medicine through Sublingual route, Application of Medicine through Respiratory Route, Application of Inhaler, Application of Ratahaler, Application of Nebulizer,
Cleaning, Dressing, Bandaging, Stitching, Oxygen Measurement, Blood Collection, Blood Grouping, Pathological Report Understanding, Prescription Understanding, Application of Ambu bag, Application of Oxygen Cylinder, Catheterization, Management of Hypertension, Management of Hypertension Emergency, Management of Diabetic Coma, Management of Shock, Management of Hypovolemic Shock, Emergency Management of Electric Shock, Emergency Management of Anaphylactic Shock, Management of Psychogenic Shock.
Anatomy and Physiology For Nursing Training Course ( NTC 1 Year) Course Fee
The study of the body’s structure by cutting organs is called Anatomy. The study of the functions of the body and its system, organs, tissues, and cells is called Physiology. Firstly our curriculum is designed with the systems. The Systems of the Human Body are the Digestive System, Respiratory System, Cardiovascular System, Endocrine System, Excretory System, Urinary System, Immune System, Lymphatic System, Male Reproductive System, Female Reproductive System, Integumentary System, Hepatobiliary System, Portal System, etc.
Then we study the Anatomy of the Digestive System, Anatomy of Tongue, Anatomy of Esophagus, Anatomy of Stomach, Anatomy of Small Intestine, Anatomy of Large Intestine, Anatomy of Cecum, Anatomy of Colon, Anatomy of Rectum, Anatomy of Anus, Anatomy of The Respiratory System, Anatomy of Nasal Concha, Anatomy of the Oropharyngeal Structure, Anatomy of the Trachea, Anatomy of the Bronchus, Anatomy of the Lung, Anatomy of the Alveolus.
Anatomy of the Heart, Anatomy of Cardiac Wall, Anatomy of Cardiac Septum, Anatomy of Cardiac Vulves, Anatomy of Blood Vessels, Anatomy of Artery, Anatomy of Vein, Anatomy of Capillary, Anatomy of Pulmonary Blood Circulation, Anatomy of Hepatic Blood Circulation, Anatomy of the Renal Blood Circulation, Anatomy of the Limbic Blood Circulation, Anatomy of the Cranial Blood Circulation, Anatomy of the Portal Blood Circulation, Anatomy of the Spleenic Blood Circulation, Anatomy of the Pancreatic Blood Circulation, Anatomy of the Coronary Blood Circulation, etc.
Pharmacology for Nursing Training Course ( NTC 1 Year) Course Fee
Key pharmacology topics include Pharmacokinetics/Dynamics, the Autonomic Nervous System (ANS) (cholinergics, anticholinergics, beta-blockers), Cardiovascular Drugs (antihypertensives, antianginals, antiarrhythmics, statins), Autacoids (NSAIDs, antihistamines, migraine meds), Antimicrobials (antibiotics, antivirals, antifungals, TB/malaria drugs), CNS Drugs (antiepileptics, local anesthetics), and Endocrine Drugs (insulin, corticosteroids, contraceptives), with general concepts like ADRs, Pharmacovigilance, and drug calculations also crucial for exams and practice.
Core Concepts
- Pharmacokinetics (PK) & Pharmacodynamics (PD): ADME (Absorption, Distribution, Metabolism, Excretion), drug interactions, therapeutic index, enzyme induction/inhibition.
- Autonomic Nervous System (ANS): Cholinergic/Anticholinergic drugs, Catecholamines, Beta-blockers, Muscarinic/Nicotinic receptors, Opiate poisoning.
- Adverse Drug Reactions (ADRs) & Pharmacovigilance: Reporting, types, teratogenicity.
System-Specific Drugs (High-Yield)
- Cardiovascular (CVS): Antihypertensives (ACEi, ARBs, CCBs), Antianginals (Nitrates), Digoxin, Antiarrhythmics (Amiodarone), Statins, Drugs for CHF.
- Respiratory: Asthma/COPD drugs, bronchodilators, antihistamines.
- Central Nervous System (CNS): Antiepileptics, Local Anesthetics, Antidepressants/Antipsychotics (general overview).
- Gastrointestinal (GIT): Antiulcer drugs (PPIs, H2 blockers), Antiemetics, Laxatives.
- Hematology: Anticoagulants, Antiplatelets, Fibrinolytics, Iron deficiency treatments.
- Endocrine: Insulin, Thyroid drugs, Corticosteroids, Contraceptives.
Antimicrobials & Chemotherapy
- Antibiotics: Cephalosporins, Penicillins, Fluoroquinolones, TB/Leprosy drugs, Antifungals, Antivirals (HAART).
- Chemotherapy: Basic principles, common agents (read lightly for general exams).
Autacoids & Inflammation
- NSAIDs & Salicylates: Mechanism, poisoning (Aspirin).
- Histamine & Antihistamines: Receptor actions, clinical uses.
General/Miscellaneous
- Drug Dosing: Loading/Maintenance doses, Clearance.
- Drug Routes: Oral, IV, IM, etc..
Study Of OTC Drugs For Nursing Training Course ( NTC 1 Year) Course Fee
The study of Over-The-Counter (OTC) drugs is a very important topic primarily because these medications are widely used for self-care, yet their potential for misuse, adverse effects, and drug interactions poses significant public health concerns. Key aspects of this subject include:
Prevalence and Motivation for Use
- High Usage: OTC drugs are used by a large percentage of the population worldwide to treat minor ailments like headaches, coughs, colds, and pain.
- Convenience and Cost: Primary reasons for self-medication include the desire to save time and money, and the ease of access without a doctor’s prescription.
- Commonly Used Drugs: Analgesics (painkillers like acetaminophen and NSAIDs), cough and cold medications (dextromethorphan), and vitamins are among the most frequently used.
Key Subject Areas and Risks
- Knowledge Gaps: Many users, including health science students and adolescents, exhibit significant gaps in their understanding of proper OTC use, including correct dosage, potential side effects, and drug interactions.
- Misuse and Addiction Potential: Certain active ingredients, such as dextromethorphan (DXM) and loperamide, have the potential for misuse at higher-than-recommended doses to achieve intoxicating effects, which can lead to addiction, overdose, and severe health problems.
- Drug Interactions: OTC medications can interact dangerously with other prescription drugs, specific foods, or alcohol, a risk often overlooked by consumers.
- Masking Symptoms: Inappropriate use of OTC drugs can mask symptoms of more serious underlying conditions, leading to delayed diagnosis and treatment.
- Specific Populations at Risk: Children and older adults require special consideration for safe use, and specific educational resources are needed for parents and caregivers.
- Misunderstanding Classifications: A significant number of people incorrectly believe antibiotics are OTC drugs, contributing to the problem of antibiotic resistance.
Regulation and Education
- Regulatory Framework: In the U.S., the FDA regulates OTC drugs through monographs, which set standards for ingredients, doses, and labeling to ensure general safety and effectiveness when used as directed.
- The Importance of the “Drug Facts” Label: The standardized label on all OTC products is a critical tool for consumers to ensure safe use, yet many people do not read it completely or correctly.
- Need for Education: Public health interventions, educational campaigns in schools, and the active involvement of pharmacists are crucial to promote responsible self-medication practices.
Studying OTC drugs is important for ensuring public safety and empowering individuals to practice self-care responsibly by understanding both the benefits and potential risks associated with these readily available medications. Consumers can find reliable information on the safe use of OTCs from resources such as the FDA and MedlinePlus.
First Aid 1 & 2 For Nursing Training Course(NTC 1 Year)
The most important topics in First Aid 1 and 2 courses focus on the immediate preservation of life and include Cardiopulmonary Resuscitation (CPR), managing severe bleeding, responding to choking, and treating for shock.
These courses, sometimes referred to as Emergency and Standard First Aid, progressively build skills to manage a wide array of life-threatening and non-life-threatening situations until professional medical help arrives.
Core Principles & Initial Response
- Scene Assessment: Ensuring the safety of yourself, bystanders, and the victim is the first priority.
- The 3 Cs (Check, Call, Care): A systematic approach to checking the scene and victim, calling emergency medical services (EMS), and providing care.
- Legal Considerations: Understanding consent and your responsibilities as a first aider, often covered by Good Samaritan laws.
- Infection Control: Using personal protective equipment (PPE) like gloves to prevent disease transmission.
Key Emergency Topics
- Cardiopulmonary Resuscitation (CPR) & AED: The most critical life-saving skill, including techniques for adults, children, and infants, and the proper use of an Automated External Defibrillator.
- Airway Emergencies & Choking: Recognizing and responding to airway obstructions using techniques like the Heimlich maneuver (abdominal thrusts) or back blows.
- Severe Bleeding: Applying direct pressure to control life-threatening external bleeding, and recognizing signs of internal bleeding.
- Shock Management: Recognizing symptoms of shock (inadequate blood flow) and taking steps to minimize its effects, such as keeping the victim warm and comfortable.
Additional Topics Covered in Level 2
Building upon basic skills, First Aid 2 (Standard First Aid) typically covers a wider range of injuries and illnesses in greater detail:
- Wound Care & Burns: Proper cleaning, dressing, and bandaging of various wounds and different degrees of burns.
- Musculoskeletal Injuries: Managing fractures, sprains, strains, and dislocations using splinting and other immobilization techniques.
- Head and Spinal Injuries: The importance of stabilizing the head and neck to prevent further damage, and knowing when not to move a victim.
- Sudden Medical Emergencies: Recognizing symptoms and providing care for conditions such as heart attacks, strokes (using the FAST acronym), seizures, asthma, diabetes, and severe allergic reactions (anaphylaxis).
- Environmental Emergencies: Responding to heat- and cold-related conditions like heatstroke and hypothermia, as well as bites, stings, and poisoning.
- Patient Transportation: Safe methods for moving a patient if necessary.
Learning and practicing these topics can equip an individual with the confidence and skills to make a difference in an emergency situation. You can find local courses and learn these vital skills through organizations like the Bangladesh Red Crescent Society or the American Red Cross.
Hematology & Pathology For Nursing Training Course(NTC 1 Year)
Hematology and Pathology are crucial, covering blood disorders (anemias, leukemia, lymphoma, bleeding/clotting issues) and general disease processes, with key topics including Anemias (Iron Deficiency, Megaloblastic, Hemolytic), Leukemias (AML, ALL, CML), Lymphomas (Hodgkin’s/NHL), Blood Bank basics, Coagulation (Hemophilia, DIC), and Morphology (smears, bone marrow), vital for diagnosing everything from infections to cancers, requiring clear understanding of lab tests, cell features (Reed-Sternberg cells, Auer rods), and molecular aspects like the Philadelphia chromosome.
Core Areas & Key Topics
Hematology (Benign & Malignant)
- Red Blood Cell Disorders: Anemias (Iron Deficiency, Megaloblastic, Hemolytic, Aplastic, G6PD Deficiency), Sickle Cell Anemia, Thalassemia.
- White Blood Cell Disorders: Leukopenia, Leukocytosis, Leukemias (AML, ALL, CML, CLL), Lymphomas (Hodgkin’s, Non-Hodgkin’s), Infectious Mononucleosis.
- Platelet Disorders: Thrombocytopenia, ITP, TTP, DIC.
- Coagulation Disorders: Hemophilia, Von Willebrand Disease (vWD), Hypercoagulability.
- Blood Transfusion: Landsteiner’s Law, Hazards, Blood Banking.
Pathology (General & Hematopathology Focus)
- General Pathology: Inflammation, Cellular Injury, Neoplasia.
- Hematopathology: Detailed study of blood & bone marrow diseases (as above).
- Lab Techniques: Peripheral smear interpretation, Bone Marrow aspiration/biopsy, Cytochemistry, Flow Cytometry, Immunohistochemistry, Liquid Biopsy.
High-Yield Concepts (Exam Focused)
- Morphology: Reed-Sternberg Cells (Hodgkin’s), Auer Rods (AML), Philadelphia Chromosome (CML).
- Pathophysiology: Erythropoiesis, Hemostasis (Primary/Secondary), RBC Metabolism.
- Clinical Correlations: How disorders manifest (e.g., anemia symptoms, bleeding risks).
These topics bridge basic science with clinical medicine, forming the bedrock for diagnosing and managing blood-related conditions, making them essential for medical exams and practice.
General Chemistry For Nursing Training Course(NTC 1 Year)
For General Chemistry, the most crucial topics form the foundation:
Atomic Structure & Periodic Trends, Chemical Bonding & Molecular Geometry, Stoichiometry (Mole Concept & Reactions), States of Matter (Gases, Liquids, Solids), Thermochemistry, Kinetics, Equilibria (Acid-Base, Solubility), Redox Reactions & Electrochemistry, and Nuclear Chemistry, as these explain matter, energy, and reactions, essential for understanding all chemistry branches.
Core Foundational Topics
- Atomic Structure & Periodic Table: Protons, neutrons, electrons, quantum numbers, electron configurations, periodic trends (ionization energy, electronegativity).
- Chemical Bonding: Ionic, covalent, metallic bonds; Lewis structures, VSEPR theory, hybridization, molecular orbital theory.
- Stoichiometry & The Mole: Molar mass, empirical/molecular formulas, balancing equations, limiting reactants, solution concentrations (molarity, molality).
- States of Matter: Gas laws (Boyle’s, Charles’s, Ideal), intermolecular forces (IMFs), properties of liquids and solids.
Key Processes & Concepts
- Thermochemistry: Enthalpy, entropy, Gibbs free energy, laws of thermodynamics, calorimetry.
- Chemical Kinetics: Reaction rates, rate laws, activation energy, collision theory, Arrhenius equation.
- Chemical Equilibria: Le Chatelier’s principle, equilibrium constants (
𝐾𝑐,
𝐾𝑝), acid-base (pH, buffers) and solubility equilibria.
- Redox & Electrochemistry: Oxidation states, balancing redox reactions, galvanic/electrolytic cells, electrode potentials.
Introduction to Other Areas
- Acids & Bases: Definitions (Arrhenius, Brønsted-Lowry), pH scale, titrations, buffer solutions.
- Nuclear Chemistry: Radioactivity, half-life, fission, fusion.
- Organic Chemistry Basics: Hydrocarbons, functional groups, basic reaction types (substitution, addition).
Mastering these topics provides a strong base for advanced study in any specific chemical field.
Cardiovascular Nursing For Nursing Training Course(NTC 1 Year)
The most important topics in cardiovascular nursing include acute coronary syndromes (ACS), heart failure, arrhythmias, and comprehensive patient assessment and education. A strong foundation in cardiovascular anatomy, physiology, and pharmacology is essential to manage these conditions effectively.
Here are the critical topics in cardiovascular nursing:
Foundational Knowledge
- Anatomy and Physiology of the Heart: Understanding the structure of the heart, blood vessels (arteries, veins, capillaries), and blood flow is fundamental to recognizing dysfunction.
- Cardiac Conduction System: Knowledge of the heart’s electrical system (SA node, AV node, etc.) is vital for interpreting electrocardiograms (ECGs) and managing rhythm disorders.
- Pharmacology: Proficiency in common cardiovascular medications, including antiarrhythmics, beta-blockers, ACE inhibitors, diuretics, and anticoagulants, is a core competency for safe practice.
Key Clinical Areas
- Cardiovascular Assessment: The ability to perform a thorough subjective (history taking) and objective (physical examination, vital signs, auscultation) assessment is crucial for early identification of problems.
- Acute Coronary Syndromes (ACS) and Myocardial Infarction (MI): Nurses must understand the pathophysiology and emergency management of conditions like unstable angina and heart attacks, including prompt intervention and post-procedure care.
- Heart Failure (HF): This is a prevalent condition requiring expert nursing care focused on symptom management, fluid balance (monitoring edema and weight gain), and patient education on diet and lifestyle modifications.
- Arrhythmias/Dysrhythmias: Recognizing and managing abnormal heart rhythms, from atrial fibrillation to life-threatening ventricular tachycardia/fibrillation, is a critical skill, often requiring expertise with monitors, defibrillators, and pacemakers.
- Hypertension and Lipid Management: Essential for preventive cardiology, this involves patient education, lifestyle counseling (diet, exercise, smoking cessation), and medication adherence to prevent further cardiovascular events.
- Cardiogenic Shock and Hemodynamic Instability: Managing critically ill patients with compromised cardiac output requires specialized knowledge of hemodynamic monitoring and interventions.
Nursing Interventions & Patient Care
- Cardiac Rehabilitation: Nurses play a significant role in guiding patients through all phases of recovery (acute, subacute, and long-term maintenance) after a cardiac event or surgery, emphasizing exercise, education, and emotional support.
- Patient Education and Lifestyle Modification: Empowering patients to manage their condition through education on diet, exercise, and symptom recognition is vital for long-term health outcomes.
- Psychosocial Support: Heart disease is stressful; providing emotional support and screening for depression/anxiety in patients and their families is an important aspect of holistic care.
These topics form the core curriculum for cardiovascular nurses, enabling them to provide comprehensive and effective care across various healthcare settings.
Gynecological Nursing For Nursing Training Course(NTC 1 Year)
Key topics in gynecological nursing include women’s health across the lifespan, common gynecological conditions, gynecological cancers, and the associated nursing management and patient education. The subject integrates clinical expertise with compassionate, woman-centred care.
Core Areas of Gynecological Nursing
Important topics often fall into the following categories:
- Anatomy and Physiology: A strong understanding of the female reproductive system, including the menstrual cycle, is foundational to the subject.
- Preventive Care & Screening: This includes the nurse’s role in promoting regular screenings like Pap tests, breast self-examinations, mammograms, and administering the HPV vaccine.
- Common Gynecological Conditions: This covers the management and nursing care for conditions such as abnormal uterine bleeding, endometriosis, pelvic inflammatory disease (PID), urinary incontinence, and ovarian cysts.
- Gynecological Cancers: Key topics include the prevention, diagnosis, treatment, and palliative care for ovarian, cervical, and breast cancers.
- Reproductive Health: This area covers contraception options, family planning, infertility management (including assisted reproductive technologies like IVF), and the ethical/legal aspects of these services.
- Menopause and Aging: Management of menopausal symptoms, hormone replacement therapy, and conditions like osteoporosis in aging women are crucial topics.
- Surgical Nursing: This involves pre- and post-operative care for gynecological procedures, from minimally invasive surgeries to hysterectomies and C-sections.
- Infections and Sexual Health: Education on sexually transmitted infections (STIs), their prevention, and syndromic case management is vital.
- Psychosocial Aspects of Care: Providing emotional support and addressing sensitive issues like mental health concerns (e.g., postpartum depression), domestic violence, and sexual assault is a critical part of the nurse’s role.
Key Skills for Gynecological Nurses
Beyond clinical knowledge, the most important skills include strong communication, cultural sensitivity, critical thinking, patient advocacy, and the ability to provide compassionate, woman-centred care.
General Nursing For Nursing Training Course(NTC 1 Year)
The most important topics in general nursing include foundational sciences like Anatomy and Physiology, core practical skills in Fundamentals of Nursing, and clinical areas such as Medical-Surgical Nursing, Pharmacology, and Ethics.
These subjects provide the essential knowledge and skills required for effective and compassionate patient care.
Foundational Sciences
A strong understanding of how the body works and the factors that affect health is crucial for a nurse.
- Anatomy and Physiology: The study of the body’s structure and how its systems and organs function together is a building block for all other medical knowledge.
- Microbiology: Understanding microorganisms, how they cause disease, and methods for infection control is vital for patient safety and preventing the spread of illness.
- Pharmacology: This subject covers medications, their effects, proper dosages, and potential adverse reactions, which is a critical responsibility for nurses.
- Pathophysiology: This course explores how disease processes affect the body at a cellular level, helping nurses understand symptoms and develop care plans.
- Nutrition and Biochemistry: Knowledge of dietary needs and the chemical reactions in the body helps nurses promote wellness and manage patient health conditions effectively.
Core Nursing Practice & Skills
These subjects focus on the direct application of nursing principles and patient interaction.
- Fundamentals of Nursing: This introductory subject covers basic nursing principles, hygiene, patient comfort, safety, and the essential steps of the nursing process (assessment, diagnosis, planning, implementation, and evaluation).
- Health Assessment: Learning how to perform thorough physical examinations and patient interviews to identify health needs is a core skill.
- Communication Skills: Effective and compassionate communication with patients, families, and the healthcare team is essential for quality care.
Specialized Clinical Areas
As students progress, the curriculum covers specific populations and health challenges.
- Medical-Surgical Nursing: This extensive subject focuses on the care of adult patients with a wide range of medical and surgical conditions.
- Community Health Nursing: Emphasizes public health, disease prevention, and health education within a community setting.
- Mental Health/Psychiatric Nursing: Prepares nurses to care for patients with mental health issues and psychiatric disorders, covering therapeutic interventions and communication techniques.
- Pediatric Nursing: Focuses on the unique care needs of infants, children, and adolescents.
- Obstetrics and Gynecological Nursing (Midwifery): Covers care for women during pregnancy, labor, delivery, and the postpartum period.
Professional and Ethical Considerations
These subjects instill the values and responsibilities inherent in the nursing profession.
Research and Evidence-Based Practice: Teaches nurses how to evaluate current research and apply the best available evidence to improve patient outcomes. Clinical Nursing For Nursing Training Course(NTC 1 Year)
Nursing Ethics and Legal Aspects: This covers the moral compass of nursing, including patient rights, confidentiality, informed consent, and professional conduct, which guides decision-making in complex situations.
Leadership and Management: Prepares nurses for coordinating care, managing teams, and navigating the healthcare system effectively.
Pediatric Nursing For Nursing Training Course(NTC 1 Year)
For pediatric nursing, crucial topics involve developmental milestones, family-centered care, effective pain management, immunization, nutrition (obesity/malnutrition), managing common childhood illnesses (asthma, infections), pediatric emergencies (trauma, poisoning, shock, fluid balance), and crucial skills like communication, psychosocial support (ADHD, autism, mental health), and technological proficiency**, all focused on unique growth stages from infancy to adolescence, notes.
Here are the most important areas:
Core Concepts & Foundations:
- Growth & Development: Understanding normal milestones (neonate to adolescent) and variations is fundamental, notes.
- Family-Centered Care: Involving parents/caregivers is essential, recognizing their vital role, notes.
- Pharmacology in Pediatrics: Dosage calculations, medication safety, and specific drug effects on growing bodies.
Clinical Skills & Management:
- Pain Assessment & Management: Using age-appropriate tools for both acute and chronic pain.
- Pediatric Emergencies: Handling shock, burns, fluid/electrolyte imbalance, poisoning, and trauma.
- Nutrition: Breastfeeding, weaning, managing obesity, malnutrition.
- Infection Control: Preventing hospital-acquired infections.
Common Conditions & Specialties:
- Immunizations: Schedules, importance, addressing concerns.
- Chronic Illness: Oncology, congenital heart defects, diabetes, asthma, autism.
- Neonatal Care: Specific needs of newborns, including critical care.
- Child Psychiatry: ADHD, mood disorders, psychosocial impacts.
Essential Nursing Focus:
- Psychosocial Support: Play therapy, emotional/mental health for sick children, coping mechanisms.
- Communication: Therapeutic communication with children and families.
- Technology: Proficiency with medical software and equipment.
These topics cover the diverse physical, psychological, and social needs unique to children, distinguishing pediatric nursing from adult care.
Orthopedic Nursing for Nursing Training Course (NTC 1 Year) Course
Orthopedic Nursing We discuss Bones of the Backbone, Bones of the Thorax, Bones of the Upper Limb, Bones of the Lower Limbs, Bones of the Head and Neck, Anatomy of a Long Bone, Anatomy of a Joint, Ligament, Tendon, Cartilage, Bone Cells, Functions of Bone Cells, Bone Matrics, Muscle, Skeletal Muscle, Smooth Muscle, Cardiac Muscle, Functions of Skeletal Muscle, Bone Fracture, Bone Disease, Cleaning, Dressing, Bandazing, Splinter, Radiology for Orthopedics, etc.
The most important topics in orthopedic nursing center on the assessment and management of musculoskeletal health, with a strong emphasis on fracture care, pain management, post-operative rehabilitation, and patient education.
Key subject areas considered essential for orthopedic nursing practice include:
Foundational Knowledge
- Musculoskeletal Anatomy and Physiology: A deep understanding of bones, joints, muscles, ligaments, and tendons, as well as the physiology of bone and fracture healing.
- Musculoskeletal Assessment: Mastering systematic assessment techniques, including neurovascular checks (the “5 Ps”: Pain, Pulse, Pallor, Paresthesia, Paralysis) to detect complications early.
- Pathophysiology of Conditions: Knowledge of common orthopedic disorders such as arthritis (osteoarthritis and rheumatoid arthritis), osteoporosis, osteomyelitis, bone tumors, and congenital disorders.
Core Clinical Practice Areas
- Fracture Management: Understanding the classification, clinical manifestations, and management of various fractures, including open fractures, stress fractures, and fragility fractures.
- Pain Management: Employing comprehensive strategies, including pharmacological (analgesics, anti-inflammatories) and non-pharmacological methods (positioning, ice/heat therapy, relaxation), to manage acute and chronic pain.
- Immobilization and Assistive Devices: Proficiency in the application and care of casts, splints, braces, and traction, and teaching patients how to use mobility aids (crutches, walkers) safely.
- Surgical Care: Involvement in perioperative nursing, including preoperative optimization, assisting during surgery, and post-operative monitoring and wound care. This includes care related to joint replacements (hip and knee arthroplasty), spinal surgeries, and trauma.
- Rehabilitation: Coordinating and facilitating the rehabilitation process with physical and occupational therapists to restore function, strength, and mobility.
Complication Prevention and Management
- Surgical Site Infection (SSI) Prevention: Adhering to strict aseptic techniques and implementing protocols for early identification and management of infections.
- Prevention of Complications: Monitoring for serious post-operative complications such as deep vein thrombosis (DVT), fat embolism, compartment syndrome, and pressure ulcers.
- Falls Prevention: Developing and implementing nurse-led programs, especially for elderly patients at risk of fragility fractures.
Patient Education and Holistic Care
- Patient Education: A crucial responsibility involves educating patients and families about conditions, treatment options, self-management strategies, and prevention of future injuries.
- Holistic Care: Addressing not just the physical injury but also the psychological and emotional impact of musculoskeletal conditions and injuries on the patient’s well-being and independence.
Practical Class on Heartbeat for Nursing Training Course ( NTC 1 Year) Course Fee
A heartbeat is the rhythmic contraction and relaxation of the heart, driven by electrical signals, pumping blood through the body; it involves phases like diastole (relaxation/filling) and systole (contraction/pumping) and is measured as beats per minute (BPM), with 60-100 BPM being a normal resting range for adults, though it varies with activity. The electrical impulse originates at the sinoatrial (SA) node, travels through the atria, and then to the ventricles, causing them to contract and pump oxygenated and deoxygenated blood.
How it works (The Cardiac Cycle)
- Diastole (Relaxation): The heart’s chambers relax, and blood flows from the body into the right atrium and from the lungs into the left atrium, then into the ventricles.
- Atrial Systole: The atria contract, pushing remaining blood into the ventricles.
- Ventricular Systole: The ventricles contract forcefully, pushing blood out: the right side sends it to the lungs, and the left side pumps it to the rest of the body.
- Cycle Repeats: The heart then re-enters diastole, refilling with blood.
Key Terms
- SA Node: The heart’s natural pacemaker, initiating the electrical signal.
- Pulse: The palpable wave of blood flow from the heart’s beat.
- Heart Rate: The number of beats per minute (BPM).
- Tachycardia: A heart rate over 100 BPM at rest.
- Bradycardia: A slow heart rate (not mentioned in snippets, but implied opposite of tachycardia).
What affects it
- Factors Such as Stress, caffeine, nicotine, exercise, and hormones can increase heart rate.
- Normal Range: 60-100 BPM at rest for most adults, though athletes often have lower rates.
Practical Class on Heart Rate for Nursing Training Course ( NTC 1 Year) Course Fee
Heart rate is the number of times your heart beats per minute (bpm), with a normal resting rate for adults generally being 60-100 bpm, though it varies with age, fitness, stress, and medications, with athletes often having lower rates. It’s a key health indicator, reflecting heart function; a consistently high rate (tachycardia, >100 bpm at rest) or low rate (bradycardia, <60 bpm at rest, unless fit) can signal issues. You can check it by feeling your pulse at the wrist or with devices, ideally after resting.
Normal Ranges & Factors
- Adults: 60-100 bpm resting.
- Athletes: Can be as low as 40 bpm or less.
- Children: Have higher rates, e.g., 80-120 bpm for ages 3-5.
- Factors Affecting It: Fitness, emotions, caffeine, alcohol, medications, illness, pregnancy, and sleep quality.
How to Check Your Heart Rate
- Rest: Sit quietly for 5-10 minutes.
- Locate Pulse: Place index and middle fingers on the thumb side of your wrist.
- Count: Count beats for 15 seconds and multiply by 4, or count for a full minute.
- Devices: Smartwatches and fitness trackers offer easy monitoring.
Practical Class on Inhaler & Rotahaler for Nursing Training Course ( NTC 1 Year) Course Fee
A practical class on inhalers and Rotahalers should focus on ensuring correct administration technique, as proper use is crucial for the medication to reach the lungs effectively.
The main important topics for a practical class include:
General Inhaler Principles
- Mechanism of Action: Understanding how inhaled medication directly targets the lungs to control conditions like asthma and COPD, and the advantages over systemic therapy.
- Importance of Correct Technique: Highlighting that poor technique is a major cause of poor disease control, and little or no medicine reaches the lungs if used incorrectly.
- Types of Inhalers: Distinguishing between different types, such as metered-dose inhalers (MDIs), dry powder inhalers (DPIs, which include the Rotahaler), and soft mist inhalers (SMIs), and when each might be appropriate for different patients.
- Common Errors: Identifying frequent mistakes, such as not exhaling fully before inhalation or not holding one’s breath afterwards.
- Patient Education: Emphasizing the need for healthcare providers to give clear verbal and demonstrated instruction, and observe the patient re-demonstrate the technique at each visit.
Specific Inhaler Technique Steps
The practical component should cover the step-by-step procedures for each device.
For Rotahaler (Dry Powder Inhaler)
- Preparation:
- Unscrew the cover and hold the Rotahaler vertically.
- Insert the capsule (Rotacap) correctly into the chamber, ensuring the clear end is in the smaller hole.
- Press the capsule firmly and rotate the base of the device to pierce and open the capsule.
- Inhalation:
- Breathe out gently and fully, away from the device.
- Place the mouthpiece in the mouth, sealing lips around it.
- Breathe in deeply and forcefully to ensure the powder is inhaled into the lungs.
- Remove the device from the mouth and hold the breath for at least 10 seconds, or as long as comfortable.
- Post-use Care:
- Check the chamber to confirm the capsule is empty.
- Discard the empty capsule shell.
- Discuss the importance of cleaning the Rotahaler and how often (e.g., every two weeks).
- Crucial Step for Steroids: If the medication is a corticosteroid, rinse or gargle the mouth with plain water and spit it out to prevent oral thrush.
For Pressurized Metered-Dose Inhaler (pMDI)
- Preparation:
- Remove the cap and shake the inhaler well before use.
- If a spacer is available, attach it, especially for patients who struggle with coordination.
- Inhalation:
- Breathe out fully, away from the inhaler.
- Place the mouthpiece in the mouth, or into the spacer.
- As the patient starts to breathe in slowly and steadily, press down on the canister to release the medication.
- Continue breathing in, then hold the breath for 5 to 10 seconds.
- Post-use Care:
- If multiple puffs are needed, wait as advised by the manufacturer/pharmacist before repeating the steps.
- Clean the MDI regularly (e.g., once a week with warm water).
- Rinse mouth after use if it contains a steroid.
Practical Class on Tachycardia for Nursing Training Course ( NTC 1 Year) Course Fee
Tachycardia is a heart rhythm disorder where the heart beats too fast, typically over 100 beats per minute (bpm) at rest in adults, signaling an electrical problem or normal response to stress, exercise, or underlying conditions like fever, anemia, anxiety, or thyroid issues, causing symptoms like palpitations, dizziness, and shortness of breath, requiring medical evaluation to determine if it’s benign (sinus tachycardia) or a serious arrhythmia needing treatment.
Types of Tachycardia
- Sinus Tachycardia: A normal response to stress, fever, or exercise, where the sinus node fires too quickly.
- Supraventricular Tachycardia (SVT): Abnormal signals start above the ventricles, causing sudden, rapid heartbeats, often felt as palpitations.
- Ventricular Tachycardia (VT): A dangerous rhythm originating in the heart’s lower chambers, potentially life-threatening.
- Atrial Fibrillation (AFib) & Flutter: Irregular, rapid heartbeats in the upper chambers (atria).
Common Symptoms
Racing heart or palpitations, Dizziness or lightheadedness, Shortness of breath, and Chest pain or discomfort.
Common Causes & Triggers
- Lifestyle: Caffeine, alcohol, stimulants, smoking, stress, lack of sleep.
- Medical Conditions: Fever, anemia, thyroid disease, dehydration, lung disease, sleep apnea, heart disease, and high blood pressure.
- Electrical Issues: Faulty heart wiring or triggers in the heart’s chambers.
Practical Class on Bradycardia for Nursing Training Course ( NTC 1 Year) Course Fee

Bradycardia is a slower-than-normal heart rate, typically under 60 beats per minute (bpm) in adults at rest, caused by issues with the heart’s electrical system, certain medications, or underlying conditions like sleep apnea or thyroid problems, leading to symptoms like dizziness, fatigue, shortness of breath, and confusion, though highly fit individuals and athletes may have a normal slow rate. Treatment varies by cause, ranging from lifestyle changes to pacemakers, and involves diagnosing the underlying problem with tools like an EKG.
What it is
- A heart rate below 60 bpm, meaning the heart isn’t pumping enough oxygen-rich blood to the body.
- Can be normal for athletes or during sleep, but problematic if it causes symptoms.
Common types
- Sinus Bradycardia: Slowing of the heart’s natural pacemaker (sinus node).
- Heart Block: Electrical signals from the upper to lower heart chambers are blocked.
Causes
- Heart Issues: Heart disease, previous heart attacks, sick sinus syndrome.
- Medications: Beta-blockers, calcium channel blockers.
- Medical Conditions: Thyroid problems, electrolyte imbalances, sleep apnea, and inflammation.
- Lifestyle: Intense physical fitness (often normal), aging.
Symptoms (when problematic)
- Dizziness, lightheadedness, fainting.
- Fatigue, weakness.
- Shortness of breath, chest pain.
- Confusion or memory problems.
Diagnosis & Treatment
- Diagnosis: Physical exam, EKG, Holter monitor, sleep study, blood tests.
- Treatment: Addressing the cause (e.g., changing meds, treating sleep apnea) or using a pacemaker for severe cases.
Practical Class on IM Injection Pushing for Nursing Training Course ( NTC 1 Year) Course Fee
The process of pushing an intramuscular (IM) injection involves a smooth, steady depression of the plunger after the needle is securely in the muscle, ensuring the medication goes in slowly to minimize discomfort, followed by quickly withdrawing the needle at the same angle and activating the safety device, then applying gentle pressure to the site with gauze. Key steps include site preparation (cleaning, Z-track method), swift 90-degree needle insertion, slow plunger push (counting to three), quick withdrawal, and immediate disposal in a sharps container.
Pre-Injection Steps (Preparation)
- Hand Hygiene & Supplies: Wash hands thoroughly and gather medication, syringe, alcohol swabs, gauze, and a sharps container.
- Site Selection & Prep: Locate the correct muscle (e.g., deltoid, ventrogluteal), clean with an alcohol swab, and let it dry.
- Z-Track Method (Optional but Recommended): Use your non-dominant hand to pull the skin and tissue to the side to prevent medication leakage into subcutaneous tissue.
- Syringe Prep: Remove the cap, ensure no large air bubbles, and tap to get a drop of medication at the tip.
The “Push” (Injection)
- Insertion: Hold the syringe like a dart and insert the needle quickly at a 90-degree angle into the muscle.
- Stabilize: Once in the muscle, use your non-dominant hand to steady the syringe.
- Depress Plunger: Slowly and steadily push the plunger all the way down, counting to three.
- Withdrawal: After the fluid is in, hold for a few seconds (around 10 for some meds), then pull the needle straight out at the same 90-degree angle.
Post-Injection Steps
- Safety: Immediately activate the needle’s safety shield and dispose of the entire syringe in the sharps container.
- Site Care: Apply gentle pressure with gauze or a cotton ball (no rubbing) and secure with a bandage if needed.
- Observe: Monitor the patient for any adverse reactions.
Process of IV Injection Pushing for Nursing Training Course ( NTC 1 Year) Course Fee
The process of IV Injection Pushing (or Bolus) involves a trained healthcare professional manually injecting medication directly into an established IV line using a syringe, following strict steps: verify order, prepare patient, scrub the IV port (clave), flush with saline to check for patency, attach the medication syringe, push the drug at a specific rate (seconds to minutes) while monitoring, and then perform a post-flush to clear the line, ensuring patient safety and proper delivery.
Key Steps in IV Push Administration
- Preparation & Verification:
- Confirm the doctor’s order, patient details, medication rights (right drug, dose, time, route, patient, documentation, reason, response).
- Gather supplies: saline flush, medication syringe, alcohol wipes, and gloves.
- Perform hand hygiene and don gloves.
- Educate the patient about the medication and potential side effects.
- Priming & Flushing (SASH Method):
- Saline Flush: Scrub the injection port (clave) with an alcohol wipe for 15-30 seconds, let it air dry, then inject 3-5mL of saline to check for patency (blood return) and clear the line.
- Medication Administration:
- Attach Medication: Attach the pre-filled medication syringe (air expelled) to the scrubbed port and twist clockwise to secure.
- Slow Push: Slowly inject the medication at the prescribed rate (e.g., over 1 minute, 2 minutes). Use a timer for accuracy; break down the volume into smaller intervals for easier pacing (e.g., 0.5mL every 30 seconds for a 1mL/min push).
- Completion (SASH):
- Follow-up Flush: After the medication, flush with another 3-5mL of saline at the same rate as the medication push to ensure all the drug enters the bloodstream and clears the tubing, preventing incompatibility with other IV fluids.
- Secure the port with a new alcohol cap if required by facility policy.
Important Considerations
- Timing is Crucial: Pushing too fast can cause adverse effects or medication waste; too slow might delay treatment.
- Compatibility: Always check if the medication is compatible with the primary IV fluid running, if any.
- Patient Monitoring: Closely watch the patient for any adverse reactions during and after administration, especially respiratory changes, notes LevelUpRN.
Practicle Class on Pulse Measurement for Nursing Training Course ( NTC 1 Year) Course Fee
The most important topics for a practical class on pulse measurement involve understanding the parameters of the pulse (rate, rhythm, and force), the technique of palpation, various pulse points, and factors influencing the reading.
Key Learning Objectives & Topics
- Anatomy and Physiology:
- Understand what pulse is (the rhythmic expansion and recoil of an artery as blood is pumped through it) and how it relates to the heartbeat (heart rate).
- Identify the major arteries used for pulse measurement (e.g., radial, carotid, brachial, femoral, etc.) and their locations.
- Measurement Technique (Palpation):
- Proper hand hygiene and patient preparation (consent, ensuring the patient is relaxed).
- Correct finger placement (using index and middle fingers, not the thumb).
- Applying appropriate pressure to feel the pulse clearly without blocking blood flow.
- Counting method: Measuring for a full 60 seconds (especially if irregular) or 30 seconds and multiplying by two if regular.
- Parameters of the Pulse:
- Rate: Normal ranges for different age groups (e.g., 60-100 bpm for healthy adults).
- Rhythm: Assessing if the beats are regular (even tempo) or irregular (regularly irregular or irregularly irregular).
- Force/Volume (Strength): Subjectively grading the pulse strength (e.g., weak/thready, normal/strong, bounding) using a scale.
- Bilateral Equality: Comparing pulses on both sides of the body (e.g., both radial pulses) to check for potential circulatory issues like arterial obstructions.
- Factors and Abnormalities:
- Discussing factors that can influence pulse rate (physical activity, emotions, age, medications, temperature, health conditions).
- Recognizing and recording abnormal findings (e.g., tachycardia, bradycardia, weak pulse in shock) and their potential clinical significance.
- Documentation:
- Accurately recording the pulse rate, rhythm, and strength in patient notes.
Practical Application
Students should practice finding and assessing pulses at various points, with the radial artery being the most common site for routine checks. The carotid pulse is important for emergency assessment, but students must learn never to palpate both carotid arteries simultaneously to avoid reducing blood flow to the brain.
Practicle Class on Nebulizer for Nursing Training Course ( NTC 1 Year) Course Fee
A practical class on nebulizers typically covers both the theoretical knowledge and the hands-on skills needed for safe and effective use. Main important topics are centered around understanding the device, proper administration technique, patient safety, and hygiene protocols.
Key Topics for a Practical Nebulizer Class
A practical class is likely to cover the following essential topics:
1. Theory and Indications
- Definition and Function: Understanding how a nebulizer converts liquid medication into a fine mist (aerosol) that can be inhaled deep into the lungs.
- Indications for Use: Identifying which respiratory conditions, such as asthma or COPD, require nebulization therapy.
- Types of Nebulizers: Distinguishing between different types (jet, ultrasonic, mesh) and their respective advantages, disadvantages, and appropriate applications.
- Medications: Learning about the various types of medications (e.g., bronchodilators, corticosteroids, mucolytics) that can be administered via nebulizer and their effects.
2. Procedure and Technique
- Preparation: Assembling the equipment (compressor, tubing, medication cup, mask/mouthpiece) and preparing the correct dose of medication.
- Patient Positioning: Ensuring the patient is in a comfortable, upright position (sitting or semi-Fowler’s) to enable maximum breathing efficiency.
- Administration Steps: A step-by-step guide to delivering the treatment effectively, including using a mouthpiece or mask correctly and encouraging slow, deep breaths through the mouth.
- Monitoring: Observing the patient during treatment for signs of improvement or adverse reactions such as palpitations, tremors, or increased difficulty breathing.
3. Safety and Maintenance
- Infection Control: Emphasizing stringent hygiene practices, including washing hands before and after treatment, and the importance of using single-use or personal equipment to prevent cross-infection.
- Cleaning and Disinfection: Proper disassembly, cleaning with soapy water, rinsing, and thorough drying of reusable parts after each use to prevent microbial growth.
- Troubleshooting: Identifying and resolving common issues, such as the machine not producing mist or unusual noises.
- Special Considerations: Adjusting the procedure for specific patient populations, such as infants, young children, or unconscious patients who may require a face mask or alternative positioning.
4. Documentation and Education
- Record Keeping: Accurately documenting the procedure, administered medication, dosage, time, and the patient’s response in their care plan or medical record.
- Patient Teaching: Instructing patients and caregivers on proper home use, maintenance, and when to report symptoms to a physician to ensure compliance and effective long-term management.
Practicle Class on Saline Infusion for Nursing Training Course ( NTC 1 Year) Course Fee
A practical class on saline infusion focuses on the core principles and procedures of intravenous fluid administration. Key topics include the indications and contraindications for use, the types of saline solutions, and the essential practical skills for administration and patient monitoring.
Core Topics for a Practical Class
1. Foundational Knowledge and Principles
- Physiology of Fluid Balance: Understanding how water and electrolytes are distributed and balanced in the body is crucial for safe fluid therapy.
- Types of IV Fluids: Differentiating between isotonic (e.g., 0.9% Normal Saline), hypotonic (e.g., 0.45% Saline), and hypertonic solutions based on their osmolarity and clinical use.
- Indications for Saline Infusion: Common uses for normal saline (0.9% NaCl) include:
- Extracellular fluid replacement (dehydration, hypovolemia, hemorrhage, sepsis).
- Treatment of metabolic alkalosis.
- Mild sodium depletion.
- Vehicle for diluting and administering compatible medications.
- Administering blood products.
- Contraindications and Cautions: Identifying conditions where saline infusion should be used with caution or avoided, such as congestive heart failure, severe renal impairment, or conditions involving sodium retention due to the risk of fluid volume overload.
2. Equipment and Preparation
- Identifying Supplies: Recognizing and preparing all necessary equipment, including IV bags, administration sets (tubing), IV cannula/catheter, tourniquet, antiseptic solution, and sterile gloves.
- Aseptic Technique: Emphasizing the mandatory use of sterile techniques throughout the procedure to prevent infection.
- Preparing the Solution and Tubing:
- Checking the IV fluid for clarity, expiry date, and any signs of contamination.
- Spiking the IV bag and priming the tubing to remove all air bubbles and prevent air embolism.
- Proper labeling of the IV bag and tubing with medication (if added), date, time, and flow rate.
3. Administration Procedure and Skills
- Patient Preparation: Explaining the procedure to the patient, obtaining consent, and ensuring a comfortable position.
- Venipuncture: Selecting an appropriate vein and inserting the IV cannula correctly.
- Calculating and Regulating Flow Rate: Learning how to manually calculate the drip rate or use an infusion pump to ensure the correct volume is delivered over the specified time.
- Troubleshooting: Addressing potential issues, such as an insufficient flow rate, pain at the injection site, or equipment failure.
4. Monitoring and Management
- Patient Monitoring: Continuously assessing the patient for signs of adverse reactions or complications, including:
- Local reactions: Pain, swelling, redness, phlebitis, or extravasation at the injection site.
- Systemic reactions: Fluid overload (peripheral/pulmonary edema, high blood pressure), electrolyte imbalances (hypernatraemia, hyponatraemia), or systemic infection.
- Documentation: Accurately recording the procedure details, including the type and amount of fluid/medication administered, flow rate, and patient response.
- When to Discontinue: Understanding the criteria for stopping the infusion and when to seek senior medical advice, especially in cases of adverse events.
Practicle Class on cannula for Nursing Training Course ( NTC 1 Year) Course Fee
A practical class on intravenous (IV) cannulation should focus on both theoretical knowledge and the hands-on skills required for safe and effective practice.
Key Theoretical Topics
- Anatomy and Physiology: Understanding the circulatory system, including differentiating between veins and arteries, and identifying suitable peripheral veins for cannulation (e.g., in the forearm, back of the hand).
- Indications and Contraindications: Knowing when IV access is necessary (e.g., for fluid administration, medication, blood transfusions, or drawing blood samples) and when it might be contraindicated (e.g., in an arm with an AV fistula or a history of breast surgery/lymph node removal).
- Cannula Selection: Learning about the different cannula sizes (gauges), their corresponding flow rates, and selecting the appropriate size based on the patient’s needs and vein condition.
- Infection Prevention and Control: Emphasizing the importance of strict aseptic non-touch technique (ANTT) to minimize the risk of infection.
- Potential Complications: Recognizing, preventing, and managing common complications such as hematoma, phlebitis, infiltration/extravasation (fluid leaking into surrounding tissue), and accidental arterial puncture.
- Documentation and Aftercare: Understanding the correct procedures for labeling the cannula site with the date/time of insertion and documenting the procedure in the patient’s records.
Essential Practical Skills
- Patient Preparation and Consent: Effectively explaining the procedure to the patient, confirming their identity, obtaining informed consent, and ensuring their comfort.
- Equipment Preparation: Assembling all necessary equipment (cannula, tourniquet, antiseptic wipes, dressing, saline flush, gloves, sharps bin) in an organized manner.
- Vein Selection and Preparation:
- Applying a tourniquet correctly.
- Identifying and palpating a suitable vein.
- Cleaning the chosen site with an antiseptic solution and allowing it to air dry.
- Insertion Technique:
- Stabilizing the vein by applying traction to the skin.
- Inserting the cannula (bevel up) at a shallow angle.
- Observing for “flashback” of blood to confirm venous entry.
- Advancing the cannula into the vein while retracting the needle (stylet) safely into its protective mechanism.
- Securing and Flushing:
- Releasing the tourniquet.
- Connecting the bionector/T-piece and flushing the cannula with saline to check for patency and signs of infiltration.
- Securing the cannula firmly with an appropriate sterile dressing, ensuring the insertion site remains visible for monitoring.
- Removal of Cannula: Learning the correct procedure for safely removing the cannula when it is no longer needed or if complications arise.
For visual examples of the procedure and equipment, you can refer to online resources and training materials (e.g., TeachMeSurgery, Ausmed).
Practicle Class on Oxygen Measurement for Nursing Training Course ( NTC 1 Year) Course Fee
A practical class on oxygen measurement covers different topics depending on whether the focus is on chemistry/environmental science (measuring oxygen in a lab or water) or biomedical/clinical science (measuring oxygen in the body).
For Biomedical/Clinical Context
The main important topics for a practical class on measuring oxygen in a clinical or physiological setting include:
- Physiology of Oxygen Transport: Understanding how oxygen is absorbed by the lungs and transported in the blood, primarily bound to hemoglobin.
- Oxygen Saturation (SpO₂) and Partial Pressure (PO₂): Defining and distinguishing between oxygen saturation (the percentage of hemoglobin carrying oxygen) and the partial pressure of oxygen in arterial blood.
- Pulse Oximetry: The core practical skill, covering the principles (spectrophotometry and light absorption differences between oxygenated and deoxygenated hemoglobin), proper use of a pulse oximeter, and factors affecting accuracy (e.g., patient movement, nail polish, tissue thickness).
- Blood Gas Analysis (BGA): An invasive but highly accurate method that provides comprehensive information, including arterial oxygen saturation (SaO₂), partial pressure of oxygen (PaO₂), pH, and carbon dioxide levels.
- Clinical Significance: Interpreting results, recognizing normal ranges (typically 95-99% SpO₂), identifying hypoxemia (low blood oxygen levels), and understanding the need for medical interventions like oxygen therapy.
- Oxygen-Hemoglobin Dissociation Curve: Understanding the relationship between PO₂ and oxygen saturation and how factors like pH and temperature shift this curve.
For Chemistry/Environmental Science Context
The main important topics for a practical class on measuring oxygen in a laboratory or environmental setting include:
- Chemical Test for Gaseous Oxygen: Performing the standard qualitative test using a glowing splint which relights in the presence of oxygen.
- Preparation of Oxygen: Practical experience with methods for generating oxygen gas, such as the catalytic decomposition of hydrogen peroxide.
- Dissolved Oxygen (DO) Measurement: Learning techniques to measure the amount of oxygen dissolved in water or other liquids, which is crucial for environmental monitoring and aquatic life.
- Winkler Method: A classic titration-based chemical method for precisely measuring dissolved oxygen (see a visual example of the setup).
- DO Meters/Probes: Using electronic meters with probes (e.g., electrochemical or optical sensors) for faster, real-time dissolved oxygen measurements in the field (see a visual example of a device).
- Applications in Industry: Discussing the use of oxygen sensors in industrial settings for combustion control, ensuring inert atmospheres, and monitoring gas purity.
 HRTD Medical Institute
HRTD Medical Institute





