Respiratory Disease and Homeopathic Treatment
Respiratory Disease. Mobile Phone Number 01969947171, 01797522136. Respiratory diseases, also known as lung diseases or pulmonary diseases, encompass a wide range of conditions that affect the airways and other structures of the lungs, impacting the ability to breathe effectively. These conditions can be acute or chronic, and can be caused by various factors, including infections, genetics, environmental exposures, and lifestyle choices. Common examples include asthma, chronic obstructive pulmonary disease (COPD), lung cancer, and pneumonia.

Common Respiratory Diseases
- Asthma: A chronic disease characterized by inflammation and narrowing of the airways, leading to symptoms like coughing, wheezing, and shortness of breath.
- COPD (Chronic Obstructive Pulmonary Disease): A group of lung diseases, including emphysema and chronic bronchitis, that cause airflow obstruction and make breathing difficult.
- Lung Cancer: A malignant tumor that can develop in the lungs, often associated with smoking and exposure to carcinogens.
- Pneumonia: An infection of the lungs that can be caused by bacteria, viruses, or fungi, leading to inflammation and fluid buildup in the air sacs.
- Bronchitis: Inflammation of the bronchial tubes, which can be acute (short-term) or chronic (long-term).
- Bronchiectasis: A condition where the airways of the lungs become widened and damaged, leading to chronic cough and infections.
- Cystic Fibrosis: A genetic disorder that affects the lungs and digestive system, causing thick, sticky mucus to build up.
- Pulmonary Fibrosis: A condition where lung tissue becomes scarred and thickened, making it difficult to breathe.
- Tuberculosis (TB): A bacterial infection that primarily affects the lungs, causing cough, fever, and weight loss.
Causes and Risk Factors of Respiratory Disease
- Infections: Viruses (like COVID-19, influenza, and RSV), bacteria, and fungi can cause respiratory infections.
- Smoking: A major risk factor for COPD, lung cancer, and other respiratory problems.
- Air Pollution: Both indoor and outdoor air pollution can irritate the lungs and contribute to respiratory diseases.
- Occupational Exposures: Exposure to dust, chemicals, and other irritants in the workplace can cause lung damage.
- Genetics: Some respiratory conditions, like cystic fibrosis, are inherited.
- Allergies: Allergic reactions can trigger asthma and other respiratory symptoms.
- Other Factors: Low birth weight, poor nutrition, and certain medical conditions can also increase the risk of respiratory problems.
Common Symptoms of Respiratory Diseases
Common symptoms of respiratory diseases include:
- Coughing (with or without mucus)
- Shortness of breath
- Wheezing
- Chest pain or tightness
- Fatigue
- Difficulty breathing during physical activity
Prevention and Management of Respiratory Diseases
- Quitting smoking: A crucial step in preventing and managing COPD and other smoking-related respiratory illnesses.
- Avoiding air pollution: Minimizing exposure to air pollutants and using air purifiers can help.
- Managing allergies: Identifying and avoiding allergens can help control asthma symptoms.
- Practicing good hygiene: Frequent handwashing and avoiding close contact with sick individuals can help prevent respiratory infections.
- Early diagnosis and treatment: Seeking medical care for respiratory symptoms can help prevent complications and improve outcomes.
- Pulmonary rehabilitation: A program that helps individuals with chronic respiratory diseases improve their breathing and exercise capacity.
Asthma: Causes, Clinical Feature, Diagnosis, Investigation, Treatment, Complication, Prevention
Asthma is a chronic respiratory disease where airways narrow and swell, making breathing difficult. Common symptoms include coughing, wheezing, shortness of breath, and chest tightness. While the exact cause is unknown, genetics and environmental factors play a role. Management involves identifying and avoiding triggers, medication, and creating an asthma action plan.
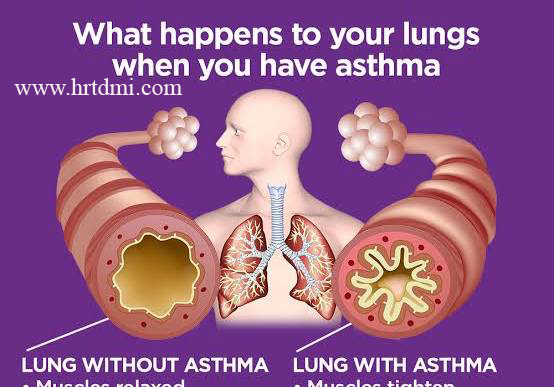
Definition: Asthma is a chronic inflammatory lung disease characterized by recurrent episodes of airflow obstruction, bronchial hyperresponsiveness, and airway inflammation.
Causes and Risk Factors of Respiratory Disease Asthma:
- Genetic Predisposition: Family history of asthma, allergies, or eczema increases risk.
- Environmental Factors: Exposure to allergens (pollen, dust mites, pet dander, mold), irritants (smoke, pollution), and respiratory infections can trigger or worsen asthma.
- Other Factors: Premature birth, low birth weight, obesity, and certain medications (beta-blockers, aspirin) are also associated with asthma.
Clinical Features of Respiratory Diseases Asthma:
- Symptoms:Wheezing, coughing (especially at night or early morning), shortness of breath, chest tightness, and difficulty breathing.
- Triggers:Allergens, exercise, cold air, infections, stress, and certain medications can trigger asthma symptoms.
Diagnosis of Respiratory Disease Asthma:
- Medical History and Physical Exam: Assess symptoms, family history, and potential triggers.
- Pulmonary Function Tests: Spirometry (measuring airflow) helps diagnose asthma and assess severity.
- Peak Expiratory Flow Rate (PEFR): Measures the maximum speed of exhalation, used for monitoring.
- Allergy Testing: May be used to identify specific allergens.
Investigations of Respiratory Disease Asthma:
- Spirometry: Measures lung function to assess airflow obstruction and reversibility.
- Allergy Skin Tests or Blood Tests: Identify specific allergens.
- Chest X-ray: May be done to rule out other lung conditions.
Treatment of Respiratory Disease Asthma:
Homeopathic Remedies that are used for the treatment of Asthma. Homeopathic Doctors will describe the uses of these homeopathic remedies widely and selectively.
| Remedy | Associated Symptoms |
|---|---|
| Arsenicum album | Wheezing, extreme weakness, anxiety, fear of disease, symptoms often worse after midnight or with cold air. |
| Pulsatilla | Wet cough with thick, yellowish phlegm, symptoms aggravated in bed, desire for company. |
| Hepar sulphuris calcareum | Dry, hoarse cough worsened by cold air and cold drinks, occurring at the beginning and end of the night. |
| Antimonium tartaricum | Wet cough with thick phlegm that is difficult to cough up, often with nausea. |
| Blatta orientalis | A specific remedy often studied for general bronchial asthma symptoms. |
| Nux vomica | Tight sensation in the chest with a dry, hacking cough, irritability, and chilliness. |
Complications of Respiratory Disease Asthma:
- Severe Asthma Attacks: Can be life-threatening if not treated promptly.
- Chronic Bronchitis: Inflammation and narrowing of the airways can lead to chronic bronchitis.
- Lung Infections: Increased susceptibility to pneumonia and other respiratory infections.
- Permanent Lung Damage: In some cases, severe asthma can cause irreversible airway damage.
Prevention of Respiratory Disease Asthma:
- Identify and Avoid Triggers: Recognize and minimize exposure to known triggers.
- Medication Adherence: Take prescribed medications as directed to prevent symptoms.
- Maintain a Healthy Lifestyle: Exercise regularly (with appropriate warm-up), maintain a healthy weight, and manage stress.
- Vaccinations: Get vaccinated against the flu and pneumonia.
- Control GERD: Manage gastroesophageal reflux disease (GERD) as it can worsen asthma symptoms.
COPD: Definition, Causes, Clinical Feature, Diagnosis, Investigation, Treatment, Complication……
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung disease characterized by persistent airflow limitation. It’s primarily caused by long-term exposure to noxious particles or gases, most commonly cigarette smoke. COPD encompasses conditions like emphysema and chronic bronchitis, leading to symptoms such as shortness of breath, chronic cough, and excessive mucus production.
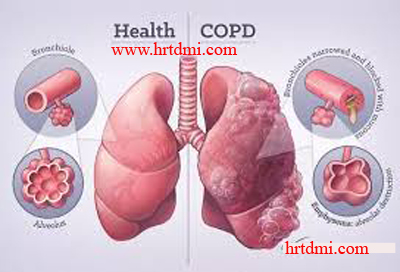
Definition: COPD is a group of lung diseases that block airflow and make it difficult to breathe. It’s not a single disease, but rather an umbrella term for conditions like emphysema and chronic bronchitis.
Causes:
- Smoking:The most common cause of COPD is long-term smoking, with the risk increasing with the number of cigarettes smoked.
- Environmental and Occupational Exposures:Exposure to air pollution, dust, fumes, and chemicals can also contribute to COPD.
- Alpha-1 Antitrypsin Deficiency:A genetic condition called alpha-1 antitrypsin deficiency can increase susceptibility to COPD, even without smoking.
Clinical Features:
- Dyspnea (Shortness of Breath): Progressive difficulty breathing, particularly during physical activity.
- Chronic Cough: A persistent cough that may produce mucus (sputum).
- Wheezing: A whistling sound during breathing.
- Chest Tightness: A feeling of pressure or constriction in the chest.
- Fatigue: Feeling unusually tired or weak.
- Weight Loss: In severe cases, COPD can lead to weight loss.
Diagnosis:
- Spirometry:This test measures lung capacity and airflow, confirming the presence of airflow obstruction.
- Medical History and Physical Examination:A doctor will assess symptoms, smoking history, and perform a physical exam.
- Imaging Tests:Chest X-rays and CT scans can help visualize lung damage and rule out other conditions.
- Arterial Blood Gas:This test measures oxygen and carbon dioxide levels in the blood.
Investigations:
- Pulmonary Function Tests (PFTs): These tests assess lung function and airflow, including spirometry.
- Chest X-ray: To visualize the lungs and identify any structural abnormalities.
- CT Scan: Provides more detailed imaging of the lungs.
- Blood Tests: To assess for alpha-1 antitrypsin deficiency and other potential causes.
Homepathic Remedies that are used for the treatment of COPD
Specific homeopathic remedies suggested in the literature for various COPD symptoms include:
- Arsenicum album: Indicated for patients with a severe barking cough (with or without mucus), chest rattling, shortness of breath, and symptoms that worsen in dry, cold, damp weather.
- Bryonia: Recommended for a dry, hacking cough with rust-colored sputum that causes stitching pain in the chest and is aggravated in warm rooms.
- Calcarea carb: Used when dyspnea worsens on exertion or climbing stairs, accompanied by ice-cold feet and a cough with greenish expectorations and chest tightness.
- Rumex: Indicated for a teasing cough that worsens in cold air, primarily affecting older adults.
- Phosphorus: Suggested for young, weak, emaciated patients who easily catch colds, have a tendency for bleeding, desire open air, and experience chest pain when lying on their left side.
- Ipecacuanha and Spongia tosta: A combination of these remedies has shown symptomatic relief in studies, particularly in reducing sputum expectoration.
- Oscillococcinum: Studies suggest that this remedy may help reduce the incidence rate and duration of upper respiratory tract infections (URTIs), which can trigger COPD exacerbations.
Complications:
- Respiratory Infections: COPD patients are more susceptible to pneumonia and other respiratory infections.
- Heart Failure: COPD can put extra strain on the heart, leading to heart failure.
- Pneumothorax: A collapsed lung can occur in severe cases.
- Respiratory Failure: In severe COPD, the lungs may not be able to provide enough oxygen or remove enough carbon dioxide, leading to respiratory failure.
Prevention:
- Quit Smoking: Avoid smoking and secondhand smoke exposure.
- Avoid Air Pollution: Minimize exposure to air pollution and other irritants.
- Vaccinations: Get vaccinated against influenza and pneumonia.
Lung Cancer: Definition, Causes, Clinical Feature (Symptoms and Signs), Treatment, etc
Lung cancer is a malignant tumor that originates in the lungs, causing uncontrolled cell growth in lung tissue. It’s a leading cause of cancer-related deaths worldwide, with smoking being the primary risk factor. Symptoms can include persistent cough, chest pain, shortness of breath, and coughing up blood. Diagnosis involves imaging, biopsies, and molecular testing. Treatment options range from surgery and radiation to chemotherapy and targeted therapies.
Definition: Lung cancer, also known as lung carcinoma, is a disease characterized by the uncontrolled growth of abnormal cells in the lungs, leading to the formation of tumors. These tumors can disrupt normal lung function and potentially spread to other parts of the body.
Causes:
- Smoking: Cigarette smoking is the leading cause of lung cancer, responsible for about 85% of cases. The harmful chemicals in cigarette smoke damage lung cells, leading to uncontrolled growth.
- Secondhand smoke: Exposure to secondhand smoke also increases the risk of lung cancer.
- Radon: Radon gas, a naturally occurring radioactive gas, is another risk factor.
- Asbestos: Asbestos exposure, particularly in occupational settings, is a known cause.
- Air pollution: Air pollution, including particulate matter, can contribute to lung cancer development.
- Other carcinogens: Exposure to other carcinogens like arsenic, cadmium, nickel, and certain other occupational substances can also increase the risk.
- Family history: Individuals with a family history of lung cancer may have a higher risk.
- HIV infection: HIV infection is also associated with an increased risk.
- Other lung diseases: Pre-existing lung diseases like pulmonary fibrosis and emphysema can also increase the risk.
Clinical Features:
- Early stages:Lung cancer can be asymptomatic in its early stages, making early detection challenging.
- Symptoms:As the cancer progresses, symptoms may include:
- Persistent cough that worsens over time
- Coughing up blood (hemoptysis)
- Chest pain that may worsen with deep breaths or coughing
- Shortness of breath
- Wheezing
- Hoarseness
- Recurrent or persistent lung infections
- Loss of appetite and weight loss
- Fatigue
- Swelling of the neck and face
- Clubbing of the fingertips and nailbeds
Diagnosis:
- Imaging:Chest X-rays, CT scans, and MRI scans are used to visualize the lungs and identify potential tumors.
- Bronchoscopy:A bronchoscopy allows for direct visualization of the airways and the collection of tissue samples.
- Biopsy:A biopsy involves removing a small sample of tissue from the tumor for microscopic examination to confirm the diagnosis and determine the type of lung cancer.
- Molecular testing:Molecular testing identifies specific genetic mutations in cancer cells, which can help guide treatment decisions.
Investigations:
- Sputum cytology: Examination of sputum for cancerous cells.
- Mediastinoscopy/EBUS: Procedures to examine lymph nodes in the mediastinum for cancer spread.
- Thoracentesis: Fluid removal from the chest cavity for analysis.
Homeopathic Remedies that are used for the treatment of Lung Cancer
Specific homeopathic remedies that have been the subject of laboratory (in vitro) and animal studies, or used in adjunct clinical trials for cancer treatment support, include:
- Sulphur: Lab studies on non-small cell lung carcinoma cells suggest that potentized Sulphur may induce cell death (apoptosis) in cancer cells while sparing normal cells.
- Thuja occidentalis: Extracts have shown anti-cancer potential in lab settings, particularly when used in photodynamic therapy against lung cancer cells.
- Ruta graveolens: In animal models (mice), this remedy has been shown to inhibit glioma (brain cancer) growth and increase the lifespan of tumor-bearing mice.
- Hydrastis canadensis and Phytolacca decandra: Extracts from these plants have demonstrated anti-cancer effects in lab studies, often through the biosynthesis of nanoparticles that induce cytotoxicity in cancer cells.
- Condurango (Marsdenia condurango): Studies in rats with induced lung cancer suggested this remedy could help ameliorate the condition by inducing apoptosis and down-regulating the epidermal growth factor receptor (EGFR) expression.
- Lycopodium clavatum: Lab studies indicate that both low and high potencies of this remedy can induce apoptosis in certain cancer cells (e.g., cervical cancer cells).
Pneumonia: Definition, Causes, Clinical Feature, Diagnosis, Investigation, Treatment, Prevention, etc.
Pneumonia is an infection that inflames the air sacs in one or both lungs, causing them to fill with fluid or pus. This inflammation can be caused by bacteria, viruses, or fungi. Common symptoms include cough with phlegm or pus, fever, chills, and difficulty breathing. Diagnosis involves physical examination, chest X-ray, and sputum analysis. Treatment typically includes antibiotics for bacterial pneumonia, and supportive care for viral pneumonia.
Definition: Pneumonia is an inflammatory condition of the lungs, primarily affecting the tiny air sacs (alveoli). These air sacs may fill with fluid or pus, leading to various respiratory symptoms.
Causes:
- Bacteria:Streptococcus pneumoniae is the most common bacterial cause, but other bacteria like Haemophilus influenzae and Mycoplasma pneumoniae can also be responsible.
- Viruses:Influenza, respiratory syncytial virus (RSV), and other viruses can cause pneumonia.
- Fungi:Fungal infections like Pneumocystis jirovecii can cause pneumonia, particularly in individuals with weakened immune systems.
Clinical Features:
- Cough: A cough that produces phlegm (mucus) is a prominent symptom. The phlegm may be green, yellow, or even bloody.
- Fever: Fever is common, often accompanied by chills.
- Shortness of Breath: Difficulty breathing or feeling breathless, especially during exertion, is a hallmark of pneumonia.
- Chest Pain: Sharp or stabbing chest pain that worsens with breathing or coughing.
- Fatigue and Weakness: Feeling unusually tired, weak, or lethargic.
- Other Symptoms: Loss of appetite, nausea, vomiting, and diarrhea can also occur.
Diagnosis:
- Medical History and Physical Examination:A doctor will inquire about your symptoms and conduct a physical exam, listening to your lungs with a stethoscope.
- Chest X-ray:This imaging test can reveal the presence and extent of lung inflammation.
- Sputum Culture:Analyzing a sample of your coughed-up mucus can help identify the specific organism causing the infection.
- Blood Tests:Blood tests can help assess the severity of the infection and identify potential complications.
Investigations:
- Pulse Oximetry: Measures the oxygen saturation in your blood.
- Arterial Blood Gas: Provides a more detailed assessment of oxygen and carbon dioxide levels in your blood.
- Complete Blood Count (CBC): Evaluates your overall blood health and helps identify signs of infection.
Homeopathic Remedies that are used for the symptomatic treatment of Pneumonia
The following are some remedies mentioned in homeopathic literature for coughs and respiratory complaints, which may include symptoms found in pneumonia.
| Remedy | Indication (Homeopathic Context) |
|---|---|
| Bryonia | Dry, painful cough, often with stitching pains in the chest, worsened by motion and relieved by rest or pressure. |
| Phosphorus | Hoarseness, tickly cough that hurts the throat, and a thirst for cold drinks. Symptoms may be worse from talking or laughing. |
| Antimonium tartaricum | Wet, rattling cough with difficulty in coughing up thick phlegm (mucus). |
| Ipecacuanha | Dry, fitful cough accompanied by nausea or vomiting, with rattling in the chest. |
| Aconitum napellus | Used in the early stages of inflammatory conditions, especially when symptoms come on suddenly after exposure to cold wind, with restlessness and fear. |
| Ferrum phosphoricum | Indicated for early stages with moderate fever, a short, tickling cough, and possibly blood-streaked mucus. |
| Pulsatilla | Wet cough with thick, yellowish phlegm, often worse at night or in a warm room. |
| Drosera | Dry, hacking, or whooping cough that comes in rapid bouts, especially worsened at night and by warmth. |
Complications:
- Respiratory Failure: Severe pneumonia can lead to respiratory failure, where the lungs are unable to provide enough oxygen to the body.
- Sepsis: In some cases, the infection can spread to the bloodstream, leading to sepsis, a life-threatening condition.
- Lung Abscess: A collection of pus can form in the lung.
- Pleural Effusion: Fluid can accumulate in the space between the lung and chest wall.
Prevention:
- Vaccination: Vaccines are available for pneumococcal pneumonia and influenza, which can significantly reduce the risk of developing these types of pneumonia.
Bronchitis: Definition, Causes, Clinical Feature, Diagnosis, Investigation, Treatment, Complication, Prevention, etc.
Bronchitis is the inflammation of the bronchial tubes, the airways that carry air to the lungs. It can be acute (short-term) or chronic (long-term). Acute bronchitis is often caused by viral infections and resolves on its own, while chronic bronchitis is usually related to smoking and is a long-term condition.
Definition:
- Bronchitis is an inflammation of the bronchial tubes, which are the airways that carry air to the lungs.
- Acute bronchitis: A short-term inflammation of the bronchial tubes, often caused by a viral infection.
- Chronic bronchitis: A long-term inflammation of the bronchial tubes, frequently associated with smoking.
Causes:
- Acute bronchitis:Primarily caused by viral infections (like the common cold or flu). Less commonly, it can be caused by bacteria or exposure to irritants like smoke or pollution.
- Chronic bronchitis:Primarily caused by smoking tobacco, but can also be triggered by long-term exposure to air pollution, dust, or other irritants.
Clinical Features:
- Symptoms: A persistent cough (often with mucus), shortness of breath, wheezing, chest discomfort, fatigue, and sometimes fever.
- Acute bronchitis: Symptoms usually last for a few weeks and improve on their own.
- Chronic bronchitis: Symptoms persist for at least three months a year for two consecutive years and can lead to chronic obstructive pulmonary disease (COPD).
Diagnosis:
- Medical history and physical exam:A doctor will ask about symptoms and medical history, and conduct a physical exam.
- Tests:Chest X-ray to rule out pneumonia, and potentially blood tests or pulse oximetry to assess oxygen levels.
Common Homeopathic Remedies for Bronchitis
The specific remedy chosen depends heavily on the type and nature of the cough and accompanying symptoms.
| Remedy | Key Symptoms and Indications |
|---|---|
| Antimonium Tartaricum | Noisy, wheezy cough with excessive mucus in the chest that is difficult to expectorate (cough up); the patient may appear bluish around the eyes/lips. |
| Bryonia Alba | Dry cough that is often painful and worsens with any movement; mucus, if present, is difficult to clear and may be rust-colored. |
| Drosera | Violent, spasmodic coughing, especially at night, which can be deep and hoarse. It is known for its anti-spasmodic effects. |
| Phosphorus | Helps manage chronic cough with a burning pain in the chest and general weakness. |
| Belladonna | Used for dry, short, harsh, and hacking coughs and spasmodic bronchitis. |
| Hepar Sulfuris | May be used to relieve bronchitis and laryngitis symptoms. |
| Spongia Tosta | Another potential option, though less detailed in the provided snippets. |
Complications:
- Acute bronchitis: May lead to pneumonia in some cases.
- Chronic bronchitis: Can progress to COPD (including emphysema), heart problems, and increased susceptibility to respiratory infections.
Prevention:
- Acute bronchitis: Vaccination against the flu and pneumonia, frequent handwashing, and avoiding close contact with sick individuals.
- Chronic bronchitis: Avoiding smoking and exposure to irritants like smoke and air pollution.
Cystic Fibrosis: Definition, Causes, Clinical Feature, Diagnosis, Investigation, Treatment, Complication, Prevention, etc.
Cystic fibrosis (CF) is a genetic disorder that primarily affects the respiratory and digestive systems due to thick, sticky mucus buildup. It’s caused by mutations in the CFTR gene, leading to a range of symptoms and complications. Diagnosis typically involves sweat tests and genetic testing, with treatment focused on managing symptoms, preventing complications, and improving quality of life.
Definition:
Cystic fibrosis is a genetic disorder caused by mutations in the CFTR gene. This gene regulates the movement of chloride and water in and out of cells, and when it’s faulty, it leads to the production of thick, sticky mucus in various organs.
Causes:
- Genetic Inheritance:Cystic fibrosis is inherited in an autosomal recessive pattern, meaning both parents must carry the mutated gene for a child to be affected.
- CFTR Gene Mutation:The CFTR gene provides instructions for making a protein that controls the movement of salt and water in and out of cells. Mutations in this gene disrupt this process, leading to thick mucus buildup.
Clinical Features:
Cystic fibrosis affects multiple organ systems, with common symptoms including:
- Respiratory System:
- Persistent cough, often with mucus production
- Wheezing and shortness of breath
- Frequent lung infections
- Nasal polyps and sinus infections
- Progressive lung damage and respiratory failure
- Digestive System:
- Greasy, foul-smelling stools
- Poor weight gain and failure to thrive in infants
- Intestinal blockages and constipation
- Pancreatitis
- Malabsorption of nutrients
- Other Symptoms:
- Salty-tasting skin
- Clubbing of fingers and toes
- Delayed puberty
- Male infertility
Diagnosis:
- Newborn Screening: Most countries screen newborns for CF using a blood spot test to check for elevated levels of immunoreactive trypsinogen (IRT), a pancreatic enzyme.
- Sweat Test:This test measures the amount of chloride in sweat, which is higher in people with CF.
- Genetic Testing:Confirms the presence of CFTR gene mutations.
- Other Investigations:Chest X-rays, sputum cultures, and stool tests can help assess the extent of lung and digestive involvement.
Complications:
- Chronic Lung Disease: Progressive lung damage, respiratory failure.
- Pancreatic Insufficiency: Malabsorption of nutrients, malnutrition.
- Liver Disease: Jaundice, liver damage.
- Infertility: Especially in males.
Prevention:
- Genetic Counseling:For families with a history of CF, genetic counseling can help assess the risk of having a child with CF.
- Carrier Testing:Testing can identify individuals who carry the mutated CFTR gene, allowing them to make informed decisions about family planning.
- Prenatal Testing:Chorionic villus sampling (CVS) or amniocentesis can detect CF in the fetus.
Pulmonary Fibrosis: Definition, Causes, Clinical Feature, Diagnosis, Investigation, Treatment, Complication, Prevention, etc.
Pulmonary fibrosis is a chronic lung disease characterized by the scarring and thickening of lung tissue, specifically around the air sacs (alveoli). This scarring makes it difficult for oxygen to pass into the bloodstream, leading to shortness of breath and other symptoms. It is a progressive disease, meaning it worsens over time.
Causes:
- Idiopathic Pulmonary Fibrosis (IPF): In many cases, the cause is unknown, and this is referred to as IPF.
- Environmental and Occupational Exposures: Exposure to certain environmental toxins, dust, and chemicals (e.g., asbestos, silica) can trigger or worsen pulmonary fibrosis.
- Medications: Some medications, like certain chemotherapy drugs, can cause lung damage and fibrosis.
- Radiation Therapy: Radiation treatment to the chest can also lead to pulmonary fibrosis.
- Autoimmune Diseases: Conditions like rheumatoid arthritis, lupus, and scleroderma can cause inflammation and scarring in the lungs.
- Other Lung Diseases: Some other lung diseases, such as sarcoidosis and certain infections, can also lead to pulmonary fibrosis.
- Genetic Predisposition: There may be a genetic component, with some individuals having a higher risk if they have a family history of pulmonary fibrosis.
- Smoking: Smoking increases the risk of developing pulmonary fibrosis.
Clinical Features:
- Shortness of Breath: This is often the first and most prominent symptom, especially with exertion.
- Dry, Hacking Cough: A persistent, non-productive cough is another common symptom.
- Fatigue and Weakness: Patients may experience fatigue, weakness, and reduced exercise tolerance.
- Chest Discomfort: Some individuals may experience chest pain or discomfort.
- Finger Clubbing: In later stages, the tips of the fingers or toes may become enlarged and rounded (clubbing).
- Rapid Weight Loss: Significant weight loss can occur, especially in advanced stages.
Diagnosis:
- Physical Examination:A doctor will listen to the lungs for crackling sounds (rales) and assess other signs and symptoms.
- Pulmonary Function Tests (PFTs):These tests measure lung capacity and how well the lungs can transfer oxygen into the bloodstream.
- High-Resolution Computed Tomography (HRCT):HRCT scans of the chest provide detailed images of the lung tissue and can show the extent of scarring.
- Bronchoscopy:A thin, flexible tube with a camera is inserted into the airways to visualize the lungs and collect samples for analysis.
- Lung Biopsy:In some cases, a small sample of lung tissue may be taken to confirm the diagnosis.
Investigations:
- Blood Tests:Blood tests may be done to rule out other conditions and assess overall health.
- Blood Gas Analysis:Measures the levels of oxygen and carbon dioxide in the blood, which can indicate the severity of lung involvement.
- Echocardiogram:This test can assess the function of the heart, as pulmonary hypertension can be a complication of pulmonary fibrosis.
Tuberculosis: Definition, Causes, Clinical Feature, Diagnosis, Investigation, Treatment, Complications, Prevention, etc.
Tuberculosis (TB) is a contagious bacterial infection, primarily affecting the lungs, but it can also impact other parts of the body. It’s caused by the bacterium Mycobacterium tuberculosis and spreads through the air when an infected person coughs, sneezes, or spits. While many people with TB infection have no symptoms (latent TB), a portion of them can develop active TB disease, which can be fatal if left untreated.
Causes:
- Mycobacterium tuberculosis: The primary cause of TB is the bacterium Mycobacterium tuberculosis.
- Airborne Transmission: The bacteria are spread through the air when an infected person coughs, sneezes, or spits.
- Crowded Environments: TB is more likely to spread in crowded, poorly ventilated indoor spaces, especially where people live or work together for extended periods, according to the Mayo Clinic.
Clinical Features:
- Latent TB:Most people infected with TB bacteria do not have symptoms and are not contagious. However, the bacteria remain dormant in the body.
- Active TB:Symptoms of active TB disease include:
- A persistent cough (lasting more than 3 weeks).
- Coughing up blood or mucus.
- Chest pain.
- Fatigue and weakness.
- Fever and night sweats.
- Loss of appetite and weight loss.
- Other symptoms can include chills, body aches, and fatigue.
Diagnosis:
- TB Skin Test (Mantoux Test): A small amount of fluid is injected under the skin, and the reaction is checked after 48-72 hours.
- TB Blood Test: Measures the immune system’s response to TB bacteria.
- Sputum Tests: Samples of sputum (phlegm) are examined for TB bacteria.
- Chest X-rays: May be used to visualize the lungs and identify any abnormalities.
- Other Tests: Depending on the suspected location of TB, tests may include urine tests or biopsies of affected tissue.
Complications:
- Drug-Resistant TB:If treatment is not completed, the bacteria can become resistant to medications.
- Organ Damage:Untreated TB can lead to damage in various organs, including the lungs, spine, kidneys, and brain.
- Skeletal TB (Pott’s Disease):TB can spread to the bones and joints, particularly the spine, causing pain, stiffness, and potential nerve damage, according to PharmEasy.
- Meningitis:TB can affect the brain and cause meningitis, a dangerous infection of the membranes surrounding the brain and spinal cord.
Prevention:
- BCG Vaccine:The Bacille Calmette-Guérin (BCG) vaccine is available to help prevent severe TB, especially in children.
- Early Detection and Treatment:Prompt diagnosis and treatment of active TB are crucial to prevent transmission.
- Preventative Therapy:People with latent TB infection may be prescribed medication to prevent them from developing active disease, according to the CDC.
- Good Ventilation:Improving ventilation in indoor spaces can help reduce the risk of TB transmission.
Bronchiectasis: Definition, Causes, Clinical Feature
Bronchiectasis is a chronic lung condition where airways become permanently widened, thickened, and damaged due to inflammation or infection, leading to excessive mucus buildup and difficulty clearing it. This excess mucus promotes recurrent infections, causing symptoms like chronic cough, excessive sputum (often yellow or green), and breathlessness. It is a long-term disease caused by factors such as severe infections (like pneumonia or tuberculosis), certain genetic conditions (such as cystic fibrosis or primary ciliary dyskinesia), immune system problems, or airway obstruction.
Clinical Features
- Chronic Productive Cough: The most common symptom is a persistent cough that produces a large amount of sputum.
- Copious Sputum: The mucus is often thick, tenacious, and can be yellow or green.
- Recurrent Infections: The trapped mucus makes the airways more susceptible to bacteria, leading to frequent lung infections.
- Breathlessness (Dyspnea): As the condition progresses and airflow is obstructed, shortness of breath can occur.
- Hemoptysis: In some cases, coughing up blood may occur.
- Localized Crackles or Wheezing: Physicians may detect abnormal sounds in the lungs during a physical examination.
Causes of Bronchiectasis
- Severe or Repeated Infections: Conditions like pneumonia, tuberculosis, measles, and COVID-19 can damage the airways and lead to bronchiectasis.
- Genetic Conditions:
- Cystic Fibrosis: A well-known genetic disorder that can cause bronchiectasis.
- Primary Ciliary Dyskinesia (PCD): A condition affecting the cilia, the tiny hair-like structures that clear mucus from the airways.
- Immune System Problems: A weakened immune system, as seen in common variable immunodeficiency, increases the risk of infections that can cause bronchiectasis.
- Airway Obstruction: Blockages, such as from a tumor or an inhaled foreign object, can lead to damage and dilation of the airways.
- Inflammatory Bowel Disease: Chronic conditions like Crohn’s disease and ulcerative colitis can sometimes be associated with bronchiectasis.
- Other Lung Conditions: Bronchiectasis can occur alongside chronic obstructive pulmonary disease (COPD) or asthma.
ব্রঙ্কাইকটেসিস হল ফুসফুসের একটি দীর্ঘস্থায়ী অবস্থা যেখানে প্রদাহ বা সংক্রমণের কারণে শ্বাসনালী স্থায়ীভাবে প্রশস্ত, ঘন এবং ক্ষতিগ্রস্ত হয়, যার ফলে অতিরিক্ত শ্লেষ্মা জমা হয় এবং তা পরিষ্কার করতে অসুবিধা হয়। এই অতিরিক্ত শ্লেষ্মা বারবার সংক্রমণের কারণ হয়, যার ফলে দীর্ঘস্থায়ী কাশি, অতিরিক্ত থুতু (প্রায়শই হলুদ বা সবুজ) এবং শ্বাসকষ্টের মতো লক্ষণ দেখা দেয়। এটি একটি দীর্ঘমেয়াদী রোগ যা গুরুতর সংক্রমণ (যেমন নিউমোনিয়া বা যক্ষ্মা), কিছু জেনেটিক অবস্থা (যেমন সিস্টিক ফাইব্রোসিস বা প্রাথমিক সিলিয়ারি ডিস্কিনেসিয়া), রোগ প্রতিরোধ ক্ষমতার সমস্যা, অথবা শ্বাসনালীতে বাধার মতো কারণগুলির কারণে ঘটে।
ক্লিনিকাল বৈশিষ্ট্য
- দীর্ঘস্থায়ী উৎপাদনশীল কাশি: সবচেয়ে সাধারণ লক্ষণ হল একটি অবিরাম কাশি যা প্রচুর পরিমাণে থুতনি তৈরি করে।
- প্রচুর কফ: শ্লেষ্মা প্রায়শই ঘন, শক্ত হয় এবং হলুদ বা সবুজ হতে পারে।
- পুনরাবৃত্ত সংক্রমণ: আটকে থাকা শ্লেষ্মা শ্বাসনালীকে ব্যাকটেরিয়ার প্রতি আরও সংবেদনশীল করে তোলে, যার ফলে ঘন ঘন ফুসফুসের সংক্রমণ হয়।
- শ্বাসকষ্ট (শ্বাসকষ্ট): অবস্থা যত এগোচ্ছে এবং বায়ুপ্রবাহ বাধাগ্রস্ত হচ্ছে, শ্বাসকষ্ট হতে পারে।
- হিমোপটিসিস: কিছু ক্ষেত্রে, কাশির সাথে রক্ত পড়তে পারে।
- স্থানীয়ভাবে কর্কশ শব্দ বা শ্বাসকষ্ট: শারীরিক পরীক্ষার সময় চিকিৎসকরা ফুসফুসে অস্বাভাবিক শব্দ সনাক্ত করতে পারেন।
ব্রঙ্কাইকটেসিসের কারণগুলি
- গুরুতর বা বারবার সংক্রমণ: নিউমোনিয়া, যক্ষ্মা, হাম এবং কোভিড-১৯ এর মতো রোগগুলি শ্বাসনালীকে ক্ষতিগ্রস্ত করতে পারে এবং ব্রঙ্কাইকটেসিসের কারণ হতে পারে।
- জিনগত অবস্থা:
- সিস্টিক ফাইব্রোসিস: একটি সুপরিচিত জেনেটিক ব্যাধি যা ব্রঙ্কাইকটেসিসের কারণ হতে পারে।
- প্রাইমারি সিলিয়ারি ডিস্কিনেসিয়া (পিসিডি): সিলিয়াকে প্রভাবিত করে এমন একটি অবস্থা, ছোট চুলের মতো গঠন যা শ্বাসনালী থেকে শ্লেষ্মা পরিষ্কার করে।
- রোগ প্রতিরোধ ক্ষমতার সমস্যা: একটি দুর্বল রোগ প্রতিরোধ ক্ষমতা, যেমনটি সাধারণ পরিবর্তনশীল ইমিউনোডেফিসিয়েন্সিতেদেখা যায় , ব্রঙ্কাইকটেসিসের কারণ হতে পারে এমন সংক্রমণের ঝুঁকি বাড়ায়।
- শ্বাসনালীতে বাধা: টিউমার বা শ্বাস-প্রশ্বাসের মাধ্যমে নেওয়া কোনও বিদেশী বস্তুর কারণে বাধার ফলে শ্বাসনালীর ক্ষতি এবং প্রসারণ হতে পারে।
- প্রদাহজনক পেটের রোগ: ক্রোন’স ডিজিজ এবং আলসারেটিভ কোলাইটিসের মতো দীর্ঘস্থায়ী অবস্থা কখনও কখনও ব্রঙ্কাইকটেসিসের সাথে যুক্ত হতে পারে।
- অন্যান্য ফুসফুসের অবস্থা: ব্রঙ্কাইকটেসিস দীর্ঘস্থায়ী অবস্ট্রাকটিভ পালমোনারি ডিজিজ (সিওপিডি) বা হাঁপানির পাশাপাশি ঘটতে পারে।
Bronchiectasis: Diagnosis, Investigation, Treatment
Bronchiectasis is diagnosed by a high-resolution CT scan, though a chest X-ray may show early signs, and confirmed by symptoms of chronic cough with mucus and repeated infections. Investigations involve sputum cultures to identify infections, spirometry for lung function, blood tests for inflammation or antibodies, and a cystic fibrosis sweat test if suspected. Treatment focuses on airway clearance techniques and physiotherapy, antibiotic therapy to treat infections, and addressing the underlying cause, with long-term antibiotics, inhaled medications, and bronchoscopy for severe or resistant cases.
Diagnosis
A medical professional will typically suspect bronchiectasis based on a patient’s history of recurrent respiratory infections and a chronic daily cough with mucus production.
- High-Resolution CT (HRCT) Scan: This is the definitive diagnostic tool, showing thickened bronchial walls and dilated airways in the lungs.
- Sputum Sample: A sample of phlegm is tested to identify bacteria, fungi, or other pathogens causing infection.
- Spirometry: This lung function test checks how well your lungs are working and may show an obstructive pattern.
Investigation for Bronchiectasis
After initial diagnosis, tests are conducted to find the underlying cause:
- Blood Tests: To check for inflammation or low immunoglobulin levels that may indicate an immune deficiency.
- Cystic Fibrosis Sweat Test: This test is performed if cystic fibrosis is suspected as the cause.
- Bronchoscopy: A flexible tube with a camera is inserted into the airways to locate blockages or infections.
- Aspergillus Skin Prick Tests: Used to detect a fungal allergy, Aspergillus.
- Alpha-1 Antitrypsin Deficiency (AATD) Screening: A blood test can screen for this genetic condition that predisposes to lung disease.
ব্রঙ্কাইকটেসিস একটি উচ্চ-রেজোলিউশন সিটি স্ক্যানের মাধ্যমে নির্ণয় করা হয়, যদিও বুকের এক্স-রে প্রাথমিক লক্ষণগুলি দেখাতে পারে এবং শ্লেষ্মা এবং বারবার সংক্রমণের সাথে দীর্ঘস্থায়ী কাশি লক্ষণগুলির দ্বারা নিশ্চিত করা যেতে পারে। তদন্তের মধ্যে রয়েছে সংক্রমণ শনাক্ত করার জন্য থুতু কালচার, ফুসফুসের কার্যকারিতার জন্য স্পাইরোমেট্রি , প্রদাহ বা অ্যান্টিবডির জন্য রক্ত পরীক্ষা এবং সন্দেহ হলেসিস্টিক ফাইব্রোসিসের ঘাম পরীক্ষা । চিকিৎসার মূল লক্ষ্য হলো শ্বাসনালী পরিষ্কারের কৌশল এবং ফিজিওথেরাপি, সংক্রমণের চিকিৎসার জন্য অ্যান্টিবায়োটিক থেরাপি এবং দীর্ঘমেয়াদী অ্যান্টিবায়োটিক, ইনহেলড ওষুধ এবং গুরুতর বা প্রতিরোধী ক্ষেত্রেব্রঙ্কোস্কোপির মাধ্যমে অন্তর্নিহিত কারণ মোকাবেলা করা।
রোগ নির্ণয়
একজন চিকিৎসা পেশাদার সাধারণত রোগীর পুনরাবৃত্ত শ্বাসযন্ত্রের সংক্রমণের ইতিহাস এবং শ্লেষ্মা উৎপাদন সহ দীর্ঘস্থায়ী দৈনিক কাশির ইতিহাসের ভিত্তিতে ব্রঙ্কাইকটেসিস সন্দেহ করেন।
- উচ্চ-রেজোলিউশন সিটি (এইচআরসিটি) স্ক্যান: এটিই হল চূড়ান্ত রোগ নির্ণয়ের হাতিয়ার, যা ফুসফুসে ঘন ব্রঙ্কিয়াল দেয়াল এবং প্রসারিত শ্বাসনালী দেখায়।
- থুতুর নমুনা: ব্যাকটেরিয়া, ছত্রাক, বা সংক্রমণ সৃষ্টিকারী অন্যান্য রোগজীবাণু সনাক্ত করার জন্য কফের একটি নমুনা পরীক্ষা করা হয়।
- স্পাইরোমেট্রি: এই ফুসফুসের কার্যকারিতা পরীক্ষাটি আপনার ফুসফুস কতটা ভালোভাবে কাজ করছে তা পরীক্ষা করে এবং একটি বাধাজনিত প্যাটার্ন দেখাতে পারে।
ব্রঙ্কাইকটেসিসের জন্য তদন্ত
প্রাথমিক রোগ নির্ণয়ের পর, অন্তর্নিহিত কারণ খুঁজে বের করার জন্য পরীক্ষা করা হয়:
- রক্ত পরীক্ষা: প্রদাহ বা কম ইমিউনোগ্লোবুলিনের মাত্রা পরীক্ষা করার জন্য যা রোগ প্রতিরোধ ক্ষমতার ঘাটতি নির্দেশ করতে পারে।
- সিস্টিক ফাইব্রোসিস ঘাম পরীক্ষা: সিস্টিক ফাইব্রোসিসের কারণ সন্দেহ হলে এই পরীক্ষাটি করা হয়।
- ব্রঙ্কোস্কোপি: বাধা বা সংক্রমণ সনাক্ত করার জন্য শ্বাসনালীতে ক্যামেরা সহ একটি নমনীয় নল ঢোকানো হয়।
- অ্যাসপারগিলাস স্কিন প্রিক টেস্ট: ছত্রাকজনিত অ্যালার্জি, অ্যাসপারগিলাস সনাক্ত করতে ব্যবহৃত হয়।
- আলফা-১ অ্যান্টিট্রিপসিন ডেফিসিয়েন্সি (AATD) স্ক্রিনিং: রক্ত পরীক্ষা এই জিনগত অবস্থার জন্য স্ক্রিন করতে পারে যা ফুসফুসের রোগের প্রবণতা তৈরি করে।
Bronchiectasis: Complication, Prevension
Complications of bronchiectasis include respiratory failure, severe bleeding from airways, recurrent infections like pneumonia, lung abscesses, and heart problems such as cor pulmonale. Prevention focuses on avoiding infections through vaccinations and good hygiene, as well as preventing initial lung damage by not smoking and avoiding exposure to secondhand smoke. Early detection and treatment of lung damage or infections can also help reduce the risk of developing bronchiectasis.
Complications of Bronchiectasis
- Respiratory Failure: If your lungs are damaged and can’t get enough oxygen to your blood, you may experience respiratory failure.
- Severe Airway Bleeding (Hemoptysis): Damaged blood vessels in the airways can rupture, leading to coughing up blood, which can be life-threatening.
- Repeated Respiratory Infections: The excess mucus in damaged airways creates an environment for bacteria to grow, leading to frequent infections.
- Lung Abscesses: In some cases, an infection can lead to a collection of pus within the lung tissue.
- Cor Pulmonale: This is a form of heart disease that develops when the heart has to work harder to pump blood through damaged lungs.
- Antibiotic Resistance: Frequent antibiotic use to treat infections can lead to resistant infections that are difficult to treat.
Prevention of Bronchiectasis
- Get Vaccinated: Routine vaccinations against diseases like measles, whooping cough, pneumonia, and influenza can prevent infections that damage the lungs.
- Avoid Smoke: Quitting smoking and avoiding exposure to secondhand smoke is crucial, as smoking can damage lung function and increase infection risk.
- Practice Good Hygiene: Maintaining good hygiene helps reduce exposure to germs and infections.
- Early Treatment of Lung Conditions: Promptly treating other lung conditions like pneumonia or COPD, as well as managing any existing lung damage, can help prevent bronchiectasis.
ব্রঙ্কাইকটেসিসের জটিলতার মধ্যে রয়েছে শ্বাসযন্ত্রের ব্যর্থতা, শ্বাসনালী থেকে তীব্র রক্তপাত, নিউমোনিয়ার মতো বারবার সংক্রমণ, ফুসফুসের ফোড়া এবং হৃদরোগ যেমন কর্পালমোনেল। প্রতিরোধের লক্ষ্য হলো টিকাদান এবং ভালো স্বাস্থ্যবিধি মেনে চলার মাধ্যমে সংক্রমণ এড়ানো, সেইসাথে ধূমপান না করে এবং পরোক্ষ ধূমপানের সংস্পর্শ এড়িয়ে প্রাথমিক ফুসফুসের ক্ষতি প্রতিরোধ করা। ফুসফুসের ক্ষতি বা সংক্রমণের প্রাথমিক সনাক্তকরণ এবং চিকিৎসা ব্রঙ্কাইকটেসিস হওয়ার ঝুঁকি কমাতেও সাহায্য করতে পারে।
ব্রঙ্কাইকটেসিসের জটিলতা
- শ্বাসযন্ত্রের ব্যর্থতা: যদি আপনার ফুসফুস ক্ষতিগ্রস্ত হয় এবং আপনার রক্তে পর্যাপ্ত অক্সিজেন না পৌঁছাতে পারে, তাহলে আপনার শ্বাসযন্ত্রের ব্যর্থতা হতে পারে।
- তীব্র শ্বাসনালী রক্তপাত (হিমোপটিসিস): শ্বাসনালীর ক্ষতিগ্রস্ত রক্তনালী ফেটে যেতে পারে, যার ফলে কাশির সাথে রক্ত বের হতে পারে, যা জীবনের জন্য হুমকিস্বরূপ হতে পারে।
- বারবার শ্বাসযন্ত্রের সংক্রমণ: ক্ষতিগ্রস্ত শ্বাসনালীতে অতিরিক্ত শ্লেষ্মা ব্যাকটেরিয়ার বৃদ্ধির জন্য পরিবেশ তৈরি করে, যার ফলে ঘন ঘন সংক্রমণ হয়।
- ফুসফুসের ফোড়া: কিছু ক্ষেত্রে, সংক্রমণের ফলে ফুসফুসের টিস্যুতে পুঁজ জমা হতে পারে।
- কর পালমোনেল: এটি হৃদরোগের একটি রূপ যা তখন বিকশিত হয় যখন ক্ষতিগ্রস্ত ফুসফুসের মধ্য দিয়ে রক্ত পাম্প করার জন্য হৃদপিণ্ডকে আরও বেশি পরিশ্রম করতে হয়।
- অ্যান্টিবায়োটিক প্রতিরোধ: সংক্রমণের চিকিৎসার জন্য ঘন ঘন অ্যান্টিবায়োটিক ব্যবহারের ফলে প্রতিরোধী সংক্রমণ হতে পারে যা চিকিৎসা করা কঠিন।
ব্রঙ্কাইকটেসিস প্রতিরোধ
- টিকা নিন: হাম, হুপিং কাশি, নিউমোনিয়া এবং ইনফ্লুয়েঞ্জার মতো রোগের বিরুদ্ধে নিয়মিত টিকাদান ফুসফুসের ক্ষতি করে এমন সংক্রমণ প্রতিরোধ করতে পারে।
- ধূমপান এড়িয়ে চলুন: ধূমপান ত্যাগ করা এবং পরোক্ষ ধূমপানের সংস্পর্শ এড়ানো অত্যন্ত গুরুত্বপূর্ণ, কারণ ধূমপান ফুসফুসের কার্যকারিতা ক্ষতিগ্রস্ত করতে পারে এবং সংক্রমণের ঝুঁকি বাড়াতে পারে।
- ভালো স্বাস্থ্যবিধি অনুশীলন করুন: ভালো স্বাস্থ্যবিধি বজায় রাখলে জীবাণু এবং সংক্রমণের সংস্পর্শ কমাতে সাহায্য করে।
- ফুসফুসের রোগের প্রাথমিক চিকিৎসা: নিউমোনিয়া বা সিওপিডিরমতো অন্যান্য ফুসফুসের রোগের তাৎক্ষণিক চিকিৎসা করা , সেইসাথে বিদ্যমান ফুসফুসের ক্ষতির ব্যবস্থাপনা, ব্রঙ্কাইকটেসিস প্রতিরোধে সাহায্য করতে পারে।
Emphysema: Definition, Clinical Feature, Causes
Emphysema is a long-term lung disease and type of COPD characterized by the progressive destruction of air sacs (alveoli), leading to shortness of breath, fatigue, and reduced lung function. Key symptoms include dyspnea (shortness of breath), a chronic cough, wheezing, and a barrel-shaped chest in advanced cases. The primary cause is chronic exposure to cigarette smoke, with other factors including exposure to industrial pollutants, air pollution, secondhand smoke, and a genetic disorder called alpha-1-antitrypsin deficiency.
Definition of Emphysema
- Emphysema is a progressive and irreversible form of chronic obstructive pulmonary disease (COPD).
- It involves the destruction and permanent enlargement of the alveoli, the tiny air sacs in the lungs responsible for oxygen and carbon dioxide exchange.
- This damage reduces the lungs’ surface area for gas exchange and impairs the ability to exhale air efficiently, leading to air trapping.
Clinical Features of Emphysema
- Shortness of breath (dyspnea), which worsens over time and with physical activity.
- Chronic cough, which may be accompanied by mucus production.
- Wheezing or a whistling sound: when breathing.
- Chest tightness .
- Fatigue and lack of energy .
- In advanced stages, individuals may develop a barrel-shaped chest, weakness, swelling in the ankles and feet, and a blue tinge to the skin (cyanosis) due to low oxygen levels.
Causes of Emphysema
- Cigarette Smoking: The most common cause, as it triggers inflammation and damages the lung tissue.
- Environmental Pollutants: Long-term exposure to certain industrial dusts, chemical fumes, and air pollution can also cause emphysema.
- Secondhand Smoke: Breathing in the smoke from others can also harm the lungs.
- Biomass Fuel Exposure: Exposure to smoke from burning wood and other organic fuels, particularly in homes, is another risk factor.
- Alpha-1-Antitrypsin Deficiency: A rare, genetic disorder where the body lacks a protective protein, making the lungs susceptible to damage.
এমফাইসেমা হল একটি দীর্ঘমেয়াদী ফুসফুসের রোগ এবং সিওপিডির ধরণ যা বায়ুথলির (অ্যালভিওলি) ক্রমশ ধ্বংসের দ্বারা চিহ্নিত, যার ফলে শ্বাসকষ্ট, ক্লান্তি এবং ফুসফুসের কার্যকারিতা হ্রাস পায়। প্রধান লক্ষণগুলির মধ্যে রয়েছে শ্বাসকষ্ট (শ্বাসকষ্ট), দীর্ঘস্থায়ী কাশি, শ্বাসকষ্ট এবং উন্নত ক্ষেত্রে পিপা আকৃতির বুক। এর প্রধান কারণ হল সিগারেটের ধোঁয়ার দীর্ঘস্থায়ী সংস্পর্শ, যার মধ্যে রয়েছে শিল্প দূষণকারী পদার্থের সংস্পর্শ, বায়ু দূষণ, পরোক্ষ ধোঁয়া এবং আলফা-১-অ্যান্টিট্রিপসিনের ঘাটতিনামক একটি জেনেটিক ব্যাধি ।
এমফিসেমার সংজ্ঞা
- এমফাইসেমা হল দীর্ঘস্থায়ী অবস্ট্রাকটিভ পালমোনারি ডিজিজ (সিওপিডি) এর একটি প্রগতিশীল এবং অপরিবর্তনীয় রূপ।
- এতে ফুসফুসের ক্ষুদ্র বায়ুথলি, যা অক্সিজেন এবং কার্বন ডাই অক্সাইড বিনিময়ের জন্য দায়ী, অ্যালভিওলির ধ্বংস এবং স্থায়ী বৃদ্ধি জড়িত।
- এই ক্ষতির ফলে ফুসফুসের গ্যাস বিনিময়ের জন্য পৃষ্ঠের ক্ষেত্রফল হ্রাস পায় এবং দক্ষতার সাথে বাতাস ত্যাগ করার ক্ষমতা ব্যাহত হয়, যার ফলে বাতাস আটকে যায়।
এমফিসেমার ক্লিনিক্যাল বৈশিষ্ট্য
- শ্বাসকষ্ট (শ্বাসকষ্ট), যা সময়ের সাথে সাথে এবং শারীরিক ক্রিয়াকলাপের সাথে আরও খারাপ হয়।
- দীর্ঘস্থায়ী কাশি, যা শ্লেষ্মা উৎপাদনের সাথে থাকতে পারে।
- শ্বাসকষ্ট বা শিসের শব্দ: শ্বাস নেওয়ার সময়।
- বুক টানটান হওয়া .
- ক্লান্তি এবং শক্তির অভাব .
- উন্নত পর্যায়ে, ব্যক্তিদের বুকে ব্যারেল আকৃতির ভাব, দুর্বলতা, গোড়ালি এবং পায়ে ফোলাভাব এবং অক্সিজেনের মাত্রা কম থাকার কারণে ত্বকে নীল আভা (সায়ানোসিস) দেখা দিতে পারে।
এমফিসেমার কারণ
- সিগারেট ধূমপান: সবচেয়ে সাধারণ কারণ, কারণ এটি প্রদাহ সৃষ্টি করে এবং ফুসফুসের টিস্যুর ক্ষতি করে।
- পরিবেশ দূষণকারী পদার্থ: নির্দিষ্ট শিল্পের ধুলো, রাসায়নিক ধোঁয়া এবং বায়ু দূষণের দীর্ঘমেয়াদী সংস্পর্শে এলে এমফিসেমা হতে পারে।
- পরোক্ষ ধোঁয়া: অন্যদের ধোঁয়া শ্বাস-প্রশ্বাসের মাধ্যমে গ্রহণ করলেও ফুসফুসের ক্ষতি হতে পারে।
- জৈববস্তুপুঞ্জ জ্বালানি এক্সপোজার: কাঠ এবং অন্যান্য জৈব জ্বালানি পোড়ানোর ধোঁয়ার সংস্পর্শে আসা, বিশেষ করে বাড়িতে, আরেকটি ঝুঁকির কারণ।
- আলফা-১-অ্যান্টিট্রিপসিনের ঘাটতি: এটি একটি বিরল, জেনেটিক ব্যাধি যেখানে শরীরে প্রতিরক্ষামূলক প্রোটিনের অভাব থাকে, যা ফুসফুসকে ক্ষতির জন্য সংবেদনশীল করে তোলে।
Emphysema: Diagnosis, Investigation, and Treatment
Emphysema is diagnosed primarily through Pulmonary Function Tests (PFTs), like spirometry, which measure lung capacity and airflow, alongside imaging tests such as CT scans and X-rays to visualize lung damage. Treatment involves addressing the root causes, such as quitting smoking, alongside therapies like oxygen therapy, inhaled medications (bronchodilators and steroids), and antibiotics for flare-ups. In severe cases, surgical options including lung volume reduction or transplant may be considered.
Diagnosis and Investigations
- Medical History and Physical Exam: Your doctor will review your medical history, inquire about smoking habits and exposure to irritants, and listen to your breathing with a stethoscope to check for signs of air trapping or wheezing.
- Pulmonary Function Tests (PFTs): These are the cornerstone of diagnosis, with spirometry measuring the amount of air your lungs can hold and how well air flows in and out.
- Imaging Tests:
- CT Scan: A CT scan provides detailed, high-resolution images of the lungs, helping to identify the extent of lung damage and rule out other conditions.
- Chest X-Ray: While less detailed than a CT scan, a chest X-ray can also help confirm a diagnosis and detect changes like hyperinflation in more severe cases.
- Arterial Blood Gas (ABG) Test: A blood test to measure the oxygen and carbon dioxide levels in your arterial blood, which assesses lung efficiency.
- Alpha-1 Antitrypsin Testing: Blood and genetic testing may be done to check for a deficiency in the alpha-1 antitrypsin protein, a genetic cause of emphysema.
Treatment
- Lifestyle Changes: Quitting smoking is crucial for slowing disease progression. Avoiding lung irritants like fumes and pollution can also help.
- Medications:
- Widly used Homeopathic Remedies will be discussed by the homeopahtic doctors.
- Oxygen Therapy: Providing supplemental oxygen can improve blood oxygen levels in severe cases.
- Supportive Therapy: Breathing assistance machines like BiPAP may be used to help with breathing.
- Surgical Options: For severe cases unresponsive to other treatments, surgery may be considered:
- Lung Volume Reduction Surgery: Removes damaged lung tissue to allow the remaining lung tissue to expand more efficiently.
- Lung Transplant: A last resort for selected patients, involving replacement of the diseased lung with a donor lung.
এমফিসেমা প্রাথমিকভাবে পালমোনারি ফাংশন টেস্ট (PFTs) এর মাধ্যমে নির্ণয় করা হয়, যেমন স্পাইরোমেট্রি, যা ফুসফুসের ক্ষমতা এবং বায়ুপ্রবাহ পরিমাপ করে, পাশাপাশি সিটি স্ক্যান এবং এক্স-রে এর মতো ইমেজিং পরীক্ষার মাধ্যমে ফুসফুসের ক্ষতি কল্পনা করা হয়। চিকিৎসার মধ্যে রয়েছে মূল কারণগুলি সমাধান করা, যেমন ধূমপান ত্যাগ করা, অক্সিজেন থেরাপি, ইনহেলড ওষুধ (ব্রোঙ্কোডাইলেটর এবং স্টেরয়েড), এবং প্রদাহের জন্য অ্যান্টিবায়োটিকের মতো থেরাপির পাশাপাশি। গুরুতর ক্ষেত্রে, ফুসফুসের পরিমাণ হ্রাস বা প্রতিস্থাপন সহ অস্ত্রোপচারের বিকল্পগুলি বিবেচনা করা যেতে পারে।
রোগ নির্ণয় এবং তদন্ত
- চিকিৎসা ইতিহাস এবং শারীরিক পরীক্ষা: আপনার ডাক্তার আপনার চিকিৎসার ইতিহাস পর্যালোচনা করবেন, ধূমপানের অভ্যাস এবং জ্বালাপোড়ার সংস্পর্শে আসার বিষয়ে জিজ্ঞাসা করবেন এবং স্টেথোস্কোপ দিয়ে আপনার শ্বাস-প্রশ্বাস শুনবেন যাতে বাতাস আটকে যাওয়া বা শ্বাসকষ্টের লক্ষণ দেখা যায় কিনা তা পরীক্ষা করা যায়।
- পালমোনারি ফাংশন টেস্ট (PFTs): এগুলো রোগ নির্ণয়ের মূল ভিত্তি, স্পাইরোমেট্রির মাধ্যমে পরিমাপ করা হয় যে আপনার ফুসফুস কতটা বাতাস ধরে রাখতে পারে এবং বাতাস কতটা ভালোভাবে ভেতরে এবং বাইরে প্রবাহিত হয়।
- ইমেজিং পরীক্ষা:
- সিটি স্ক্যান: একটি সিটি স্ক্যান ফুসফুসের বিস্তারিত, উচ্চ-রেজোলিউশনের ছবি প্রদান করে, যা ফুসফুসের ক্ষতির পরিমাণ সনাক্ত করতে এবং অন্যান্য অবস্থার সম্ভাবনা বাদ দিতে সাহায্য করে।
- বুকের এক্স-রে: সিটি স্ক্যানের তুলনায় কম বিস্তারিত হলেও, বুকের এক্স-রে রোগ নির্ণয় নিশ্চিত করতে এবং আরও গুরুতর ক্ষেত্রে হাইপারইনফ্লেশনের মতো পরিবর্তন সনাক্ত করতেও সাহায্য করতে পারে।
- ধমনী রক্ত গ্যাস (ABG) পরীক্ষা: আপনার ধমনী রক্তে অক্সিজেন এবং কার্বন ডাই অক্সাইডের মাত্রা পরিমাপ করার জন্য একটি রক্ত পরীক্ষা, যা ফুসফুসের কার্যকারিতা মূল্যায়ন করে।
- আলফা-১ অ্যান্টিট্রিপসিন পরীক্ষা: এমফিসেমার জিনগত কারণ, আলফা-১ অ্যান্টিট্রিপসিন প্রোটিনের ঘাটতি পরীক্ষা করার জন্য রক্ত এবং জেনেটিক পরীক্ষা করা যেতে পারে।
চিকিৎসা
- জীবনযাত্রার পরিবর্তন: রোগের অগ্রগতি ধীর করার জন্য ধূমপান ত্যাগ করা অত্যন্ত গুরুত্বপূর্ণ। ধোঁয়া এবং দূষণের মতো ফুসফুসের জ্বালাপোড়া এড়িয়ে চলাও সাহায্য করতে পারে।
- ওষুধ:
- হোমিওপ্যাথিক ডাক্তাররা বহুল ব্যবহৃত হোমিওপ্যাথিক প্রতিকার নিয়ে আলোচনা করবেন।
- অক্সিজেন থেরাপি: গুরুতর ক্ষেত্রে সম্পূরক অক্সিজেন সরবরাহ করলে রক্তে অক্সিজেনের মাত্রা উন্নত হতে পারে।
- সহায়ক থেরাপি: শ্বাস-প্রশ্বাসে সাহায্য করার জন্য BiPAP-এর মতো শ্বাস-প্রশ্বাসের সহায়ক যন্ত্র ব্যবহার করা যেতে পারে।
- অস্ত্রোপচারের বিকল্প: অন্যান্য চিকিৎসার প্রতি সাড়া না দেওয়া গুরুতর ক্ষেত্রে, অস্ত্রোপচার বিবেচনা করা যেতে পারে:
- ফুসফুসের ভলিউম হ্রাস সার্জারি: ক্ষতিগ্রস্ত ফুসফুসের টিস্যু অপসারণ করে যাতে অবশিষ্ট ফুসফুসের টিস্যু আরও দক্ষতার সাথে প্রসারিত হয়।
- ফুসফুস প্রতিস্থাপন: নির্বাচিত রোগীদের জন্য একটি শেষ অবলম্বন, যার মধ্যে রয়েছে রোগাক্রান্ত ফুসফুসকে দাতার ফুসফুস দিয়ে প্রতিস্থাপন করা।
Emphysema: Complication, and Prevention
Emphysema complications include lung collapse (pneumothorax), cor pulmonale (heart failure), severe respiratory infections like pneumonia, anxiety, depression, and an increased risk of lung cancer. Prevention focuses on avoiding irritants, particularly not smoking and avoiding secondhand smoke, as well as protecting your lungs from chemical fumes and air pollution.
Complications of Emphysema
- Pneumothorax (Collapsed Lung): Large air pockets in the lungs can burst, causing air to leak into the space around the lung, leading to its collapse and potentially life-threatening situations.
- Cor Pulmonale: Damage to the lungs and reduced oxygen levels can strain the heart, leading to high blood pressure in the arteries between the heart and lungs, which causes the right side of the heart to enlarge and weaken.
- Pneumonia and other Respiratory Infections: Weakened lungs are more susceptible to infections, such as pneumonia and bronchitis, which can be severe.
- Lung Cancer: People with emphysema, especially smokers, have an increased risk of developing lung cancer.
- Anxiety and Depression: The chronic breathing difficulties and limitations imposed by emphysema can negatively impact mental health.
- Increased Risk of Other Conditions: Complications can also include osteoporosis, fractures, type 2 diabetes, and gastroesophageal reflux.
- Respiratory Failure: In severe cases, emphysema can progress to respiratory failure, where the lungs can no longer provide enough oxygen to the body.
Prevention of Emphysema
- Don’t Smoke: Quitting smoking is the most important step to prevent emphysema or slow its progression. Avoid all forms of tobacco, including e-cigarettes and vaping products.
- Avoid Secondhand Smoke: Stay away from others’ smoke to protect your lungs.
- Protect Yourself from Air Pollutants: Wear protective masks and take other safety measures if you work with chemical fumes, dust, or vapors.
- Avoid Air Pollution: Minimize exposure to air pollution and other irritants when possible.
- Get Vaccinated: Stay up-to-date on your flu and pneumococcal vaccines to reduce the risk of serious respiratory infections.
এমফিসেমার জটিলতার মধ্যে রয়েছে ফুসফুস ধসে পড়া (নিউমোথোরাক্স), কর্পালমোনেল (হৃদযন্ত্রের ব্যর্থতা), নিউমোনিয়ার মতো গুরুতর শ্বাসযন্ত্রের সংক্রমণ, উদ্বেগ, বিষণ্নতা এবং ফুসফুসের ক্যান্সারের ঝুঁকি বৃদ্ধি। প্রতিরোধের লক্ষ্য হলো জ্বালাময়ী পদার্থ এড়িয়ে চলা, বিশেষ করে ধূমপান না করা এবং পরোক্ষ ধোঁয়া এড়িয়ে চলা, সেইসাথে রাসায়নিক ধোঁয়া এবং বায়ু দূষণ থেকে আপনার ফুসফুসকে রক্ষা করা।
এমফিসেমার জটিলতা
- নিউমোথোরাক্স (ফুসফুস ভেঙে যাওয়া): ফুসফুসের বড় বড় বায়ু পকেট ফেটে যেতে পারে, যার ফলে ফুসফুসের চারপাশের স্থানে বাতাস ঢুকে যেতে পারে, যার ফলে ফুসফুস ভেঙে যেতে পারে এবং সম্ভাব্য জীবন-হুমকির পরিস্থিতি তৈরি হতে পারে।
- কর পালমোনেল: ফুসফুসের ক্ষতি এবং অক্সিজেনের মাত্রা কমে যাওয়ার ফলে হৃদপিণ্ডের উপর চাপ পড়তে পারে, যার ফলে হৃদপিণ্ড এবং ফুসফুসের মধ্যবর্তী ধমনীতে উচ্চ রক্তচাপ দেখা দেয়, যার ফলে হৃদপিণ্ডের ডান দিকটি বড় এবং দুর্বল হয়ে যায়।
- নিউমোনিয়া এবং অন্যান্য শ্বাসযন্ত্রের সংক্রমণ: দুর্বল ফুসফুস নিউমোনিয়া এবং ব্রঙ্কাইটিসের মতো সংক্রমণের জন্য বেশি সংবেদনশীল, যা মারাত্মক হতে পারে।
- ফুসফুসের ক্যান্সার: এমফিসেমায় আক্রান্ত ব্যক্তিদের, বিশেষ করে ধূমপায়ীদের, ফুসফুসের ক্যান্সার হওয়ার ঝুঁকি বেশি থাকে।
- উদ্বেগ এবং বিষণ্ণতা: এমফিসেমার কারণে দীর্ঘস্থায়ী শ্বাসকষ্ট এবং সীমাবদ্ধতা মানসিক স্বাস্থ্যের উপর নেতিবাচক প্রভাব ফেলতে পারে।
- অন্যান্য অবস্থার ঝুঁকি বৃদ্ধি: জটিলতার মধ্যে অস্টিওপোরোসিস, ফ্র্যাকচার, টাইপ 2 ডায়াবেটিস এবং গ্যাস্ট্রোইসোফেজিয়াল রিফ্লাক্সও অন্তর্ভুক্ত থাকতে পারে।
- শ্বাসযন্ত্রের ব্যর্থতা: গুরুতর ক্ষেত্রে, এমফিসেমা শ্বাসযন্ত্রের ব্যর্থতায় পরিণত হতে পারে, যেখানে ফুসফুস আর শরীরকে পর্যাপ্ত অক্সিজেন সরবরাহ করতে পারে না।
এমফিসেমা প্রতিরোধ
- ধূমপান করবেন না: এমফিসেমা প্রতিরোধ বা এর অগ্রগতি ধীর করার জন্য ধূমপান ত্যাগ করা সবচেয়ে গুরুত্বপূর্ণ পদক্ষেপ। ই-সিগারেট এবং ভ্যাপিং পণ্য সহ সকল ধরণের তামাক এড়িয়ে চলুন।
- পরোক্ষ ধূমপান এড়িয়ে চলুন: আপনার ফুসফুসকে সুরক্ষিত রাখতে অন্যের ধোঁয়া থেকে দূরে থাকুন।
- বায়ু দূষণকারী পদার্থ থেকে নিজেকে রক্ষা করুন: রাসায়নিক ধোঁয়া, ধুলো বা বাষ্প নিয়ে কাজ করলে প্রতিরক্ষামূলক মুখোশ পরুন এবং অন্যান্য সুরক্ষা ব্যবস্থা গ্রহণ করুন।
- বায়ু দূষণ এড়িয়ে চলুন: সম্ভব হলে বায়ু দূষণ এবং অন্যান্য জ্বালাপোড়ার সংস্পর্শ কমিয়ে আনুন।
- টিকা নিন: গুরুতর শ্বাসযন্ত্রের সংক্রমণের ঝুঁকি কমাতে আপনার ফ্লু এবং নিউমোকোকাল টিকা সম্পর্কে হালনাগাদ থাকুন।
 HRTD Medical Institute
HRTD Medical Institute




