RMP Course/Rural Medical Practitioner Details
RMP Course/Rural Medical Practitioner. Mobile Phone Number 01797522136, 01987073965. RMP Course is a short medical course. RMP Course/Rural Medical Practitioner is the short form of Rural Medical Practitioner Course. The duration of this course is 6 Months and 1 Year.

The course fee for RMP Course/Rural Medical Practitioner 6 Months is Tk 26500/-, and RMP 1 Year Tk 52500/-. 6 Months contains 5 subjects and 1 year includes 10 subjects. The subjects are human anatomy and physiology, pharmacology, first aid, study of OTC drugs, hematology and pathology, microbiology, antimicrobial drugs, practice of medicine, etc. RMP Course 6 Months, and RMP Course 1 Year are available at HRTD Medical Institute.
Location of RMP Course/Rural Medical Practitioner
Location of RMP Course/Rural Medical Practitioner. HRTD Medical Institute, Abdul Ali Madbor Mansion, Section-6, Block-Kha, Road-1, Plot-11, Metro Rail Piller No. 249, Mirpur-10 Golchattar, Dhaka-1216.

Qualification for Admission into the Rural Medical Practitioner
Qualification for RMP Course/Rural Medical Practitioner. Minimum Qualification for Admission is SSC Pass. However, HSC, Bachelor Degree Pass, and Master Degree Pass students can be admitted into the RMP Course.
Subjects for the Rural Medical Practitioner Course
Subject for RMP Course/Rural Medical Practitioner. The subjects are human anatomy and physiology, pharmacology, first aid, the study of OTC drugs, hematology and pathology, microbiology and antimicrobial drugs, and the practice of medicine.
Subjects for Long RMP Course
Subject for RMP Course/Rural Medical Practitioner :
Human Anatomy & Physiology
Pharmacology
Study of OTC Drugs & Medicine
General First Aid
Microbiology & Antimicrobial Drugs
Hematology & Pathology
Practice of Medicine
Medical Diagnosis
Primary General Surgery
Primary Midwifery
Cardiovascular Anatomy & Physiology
Orthopedic Anatomy & Physiology
Common Cardiovascular Diseases
Common Orthopedic Diseases
Common Gynecological Diseases
Common Respiratory Diseases
Common Pediatric Problems and Proper Management
Primary Gastrology for Long RMP Course
Why RMP Courses are Important?
মহান আল্লাহ রাব্বুল আলআমিন মানুষকে যে জীবন দান করেছেন তার ধারক হিসেবে দিয়েছেন দেহকে । এই দেহকে ভালোভাবে জানতে পারা, এর পরিচর্যা করা, রক্ষনাবেক্ষন করতে পারা প্রত্যেকটি মানুষের জন্য ফরজ বলে আমি মনে করি । একজন ড্রাইভার যদি ড্রাইভিং এর পাশাপাশি তার গাড়ির প্রাথমিক পরিচর্যা, রক্ষনাবেক্ষন না করতে পারে তবে তাকে মাঝে মাঝে বড় ধরনের সমস্যায় পড়তেই হবে । আর যদি গাড়ির পরিচর্যা, প্রাথমিক মেকানিক, রক্ষনাবেক্ষন ইত্যাদি বিষয়ে জ্ঞান অর্জন করে, দক্ষতা এবং অভিজ্ঞতা অর্জন করে, তবে পথের মাঝে গাড়ি নষ্ট হলেও সে প্রাথমিক ভাবে সারিয়ে নিতে পারবে এবং পরবর্তিতে গাড়ি ড্রাইভ করে ভালো মানের ইন্জিনিয়ারিং সোপে নিয়ে গাড়ি ঠিক করে নিতে পারবে ।
একজন মানুষের ক্ষেত্রেও ঠিক তেমনি । দেহ সম্পকে জ্ঞান, দেহের প্রাথমিক পরিচর্যা, দেহের রক্ষনাবেক্ষন, দেহের প্রাথমিক চিকিৎসা ইত্যাদি বিষয়ে জ্ঞান, দক্ষতা এবং অভিজ্ঞতা অর্জন করলে সারাটা জীবন দেহটাকে সুন্দরভাবে পরিচালনা করা যায়, বেশি অসুস্থ্য হলে সঠিক সময়ে সঠিক ডাক্তারের কাছে গিয়ে সঠিক চিকিৎসা নেয়া যায় ।
Almighty Allah Rabbul Alamin has given the body as the container of the life He has given to man. I think it is a duty for every human being to know this body well, take care of it, and protect it.If a driver is not able to take basic care and maintenance of his car along with driving, then he has to face big problems at times.And if he acquires knowledge, skills and experience in car maintenance, basic mechanics, maintenance, etc., even if the car breaks down on the way, he can fix it initially and later drive the car and fix the car with good quality engineering soap.
The same is the case with a human being. If you acquire knowledge, skills and experience about the body, basic care of the body, maintenance of the body, basic treatment of the body, you can manage the body beautifully throughout your life, if you are very sick, you can go to the right doctor at the right time and get the right treatment.
Practical Class for Rural Medical Practitioner/RMP Course
Regularly Practical Class. Practical Classes are Anatomy Practical Class, Digestive System, Respiratory System, Cardiovascular System, Reproductory System, Urinary System, Endocrine System, Nervous System, Scalatel System, Muscular System, Lymphatic System, Heart, Brain, Lung, Kidney, Liver, Stomach, Spleen, Uterus, Vagina, Testis, Ovary, etc.
General Practical Classes are Heart Beat, Atrial Beat, Ventricular Beat, Heart Rate, Arrhythmia, Tachycardia, Bradycardia, Pulse, Pulse Rate, Shock, Injection Pushing, IM Injection Pushing, IV Injection Pushing, Saline Pushing, SC Injection Pushing, ID Injection Pushing, Blood Pressure, Systolic Blood Pressure, Diastolic Blood Pressure, Pulse Pressure, Mean Blood Pressure, Hypertension, Mild Hypertension, Moderate Hypertension, Severe Hypertension, Hypertension Emergency, Cleaning, Dressing, Bandaging, Stitching, Respiratory Meter, Oxygen Inhalation, Nebulizer, Rotahaler, Inhaler, Pulse Oximeter, Saturated Oxygen, etc.
সাধারণ ব্যবহারিক ক্লাস হল হার্ট বিট, অ্যাট্রিয়াল বিট, ভেন্ট্রিকুলার বিট, হার্ট রেট, অ্যারিথমিয়া, টাকাইকার্ডিয়া, ব্র্যাডিকার্ডিয়া, পালস, পালস রেট, শক, ইনজেকশন পুশিং, আইএম ইনজেকশন পুশিং, আইভি ইনজেকশন পুশিং, স্যালাইন পুশিং, এসসি ইনজেকশন পুশিং, আইডি ইনজেকশন পুশিং , রক্তচাপ, সিস্টোলিক রক্তচাপ, ডায়াস্টোলিক রক্তচাপ, পালস প্রেসার, গড় রক্তচাপ, উচ্চরক্তচাপ, হালকা উচ্চ রক্তচাপ, মাঝারি উচ্চ রক্তচাপ, গুরুতর উচ্চ রক্তচাপ, উচ্চ রক্তচাপ জরুরী, পরিষ্কার করা, ড্রেসিং, ব্যান্ডেজিং, সেলাই, রেসপিরেটরি মিটার, অক্সিজেন ইনহেলেশন, নেবুলাইজার, রোটালসমিটার, রোটালজিন, লোমকার্ড ইত্যাদি
Teacher for RMP Course/Rural Medical Practitioner
Dr. Sakulur Rahman, MBBS, CCD
Dr. Amena Afroze Anu, MBBS, PGT
Dr. Benzir, MBBS,
Dr. Disha, MBBS,
Dr. Tisha, MBBS, PGT
Dr. Shamima, MBBS, PGT
Dr. Mahinul, MBBS
Dr. Turzo, MBBS
Dr. Rejoan Rana, MBBS
Dr. Sanjana, BDS
Dr, Nazmun Nahar Juthi, BDS
Dr. Kamrunnahar Keya, BDS
Dr. Lamia, MBBS
Class Time for RMP Course/Rural Medical Practitioner
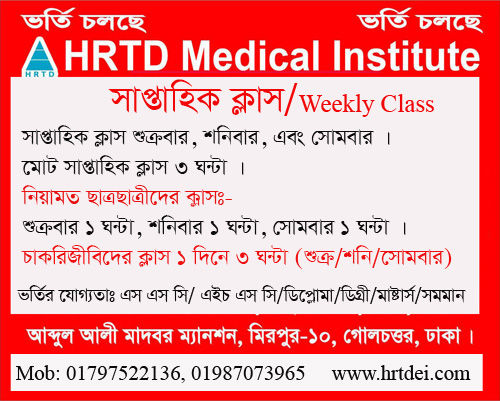
Weekly Class 3 hours. For Regular Students Friday 1 hour, Saturday 1 hour, and Monday 1 hour. For Job holders, Friday is 3 hours, or Monday is 3 hours. Morning Shift 9:00 am to 12:00 pm, and Evening Shift 3:00 pm to 6:00 pm.
Anatomy and Physiology for RMP Course/Rural Medical Practitioner
Anatomy & Physiology (A&P) covers the body’s structure (Anatomy) and function (Physiology) from cells to systems, with main topics including Cell Biology, Tissues, Homeostasis, and the Major Organ Systems (Integumentary, Skeletal, Muscular, Nervous, Endocrine, Cardiovascular, Lymphatic, Respiratory, Digestive, Urinary, Reproductive), focusing on how they work together for health and disease, using both microscopic (histology) and macroscopic (regional/systemic) approaches.
Core Concepts
- Introduction: Levels of organization (cells, tissues, organs, systems), Homeostasis & Feedback loops.
- Cytology & Histology: Cells, membranes, basic tissue types (epithelial, connective, muscle, nervous).
Major Organ Systems (Anatomy & Physiology)
- Integumentary System: Skin, hair, nails, thermoregulation.
- Skeletal System: Bones, joints, cartilage (Osteology).
- Muscular System: Muscles, contraction, movement.
- Nervous System: Brain, spinal cord, nerves, senses, nerve impulse transmission.
- Endocrine System: Hormones, glands, regulation.
- Cardiovascular System: Heart, blood, vessels, circulation, ECG, BP.
- Respiratory System: Lungs, gas exchange, breathing mechanics.
- Digestive System: Tract, accessory organs, nutrient absorption.
- Urinary System: Kidneys, urine formation, fluid balance.
- Reproductive System: Male & female structures and functions.
- Lymphatic System & Immunity: Lymph nodes, spleen, immune response.
Key Approaches
- Microscopic Anatomy: Cells, tissues (Histology).
- Macroscopic Anatomy: Regional (head, limbs, trunk) or Systemic (by system).
- Comparative Anatomy: Comparing structures across species (less common in basic A&P).
Pharmacology for RMP Course/Rural Medical Practitioner
Pharmacology main topics cover General Principles (Pharmacokinetics: ADME – Absorption, Distribution, Metabolism, Excretion; Pharmacodynamics: Drug Action/Mechanism) and Systemic/Specialized Pharmacology (Autonomic NS, CNS, Cardiovascular, Antimicrobials, etc.), focusing on how drugs affect the body (drug action) and how the body processes drugs (drug disposition) for therapeutic or harmful effects, including drug development, safety (toxicology, pharmacovigilance), and clinical use.
I. General Pharmacology (Foundational Concepts)
- Introduction: Scope, definitions, drug nomenclature, sources.
- Pharmacokinetics (ADME): How the body handles drugs.
- Absorption: Routes of administration, barriers, factors.
- Distribution: Volume of distribution (Vd), plasma protein binding.
- Metabolism (Biotransformation): Liver enzymes, induction/inhibition.
- Excretion: Elimination routes.
- Pharmacodynamics: How drugs affect the body.
- Drug-receptor interactions, dose-response, selectivity.
- Adverse Drug Reactions (ADRs) & Interactions: Recognizing side effects, polypharmacy issues.
- Drug Development & Regulation: Drug discovery, clinical trials, pharmacovigilance.
II. Specific/Systemic Pharmacology (Drug Classes & Systems)
- Autonomic Nervous System (ANS) Pharmacology: Drugs affecting the SNS & PNS.
- Central Nervous System (CNS) Pharmacology: Sedatives, antipsychotics, antidepressants, etc..
- Cardiovascular Pharmacology: Antihypertensives, antiarrhythmics, etc.
- Antimicrobial Agents: Antibiotics, antivirals, antifungals.
- Endocrine Pharmacology: Hormones, antidiabetics.
- Respiratory & Gastrointestinal Pharmacology.
- Hematology & Oncology Drugs.
III. Related & Applied Areas
- Clinical Pharmacology: Rational drug use in patients, pharmacotherapy.
- Toxicology: Poisoning and antidotes.
- Pharmacognosy: Natural products.
- Pharmaceutical Care: Patient-centered drug therapy.
These topics build from fundamental principles to specific drug applications, crucial for medicine and pharmacy.
First Aid for RMP Course/Rural Medical Practitioner
The main topics for a standard First Aid Level 1 or Basic First Aid subject generally cover the essential skills needed to manage immediate life-threatening situations and common injuries until professional medical help arrives.
Key topics include:
- Scene Assessment and Safety: Ensuring the environment is safe for both the first aider and the casualty before taking action.
- Primary Survey (Initial Assessment): Quickly checking for life-threatening conditions using a systematic approach like the DRSABCD Action Plan (Danger, Response, Send for help, Airway, Breathing, CPR, Defibrillation).
- Cardiopulmonary Resuscitation (CPR): Techniques for performing CPR on adults, children, and infants, and the use of an Automated External Defibrillator (AED).
- Airway Management: Techniques for opening and maintaining an airway, including managing choking victims.
- Severe Bleeding Control: Methods to control various types of bleeding, which is crucial as uncontrolled bleeding can be life-threatening.
- Shock Management: Recognizing the signs and symptoms of shock (a life-threatening condition that occurs when the body is not getting enough blood flow) and how to manage it.
- Wound Care: Cleaning and dressing minor wounds and injuries.
- Burns: Recognizing the types and severity of burns and applying appropriate first aid.
- Musculoskeletal Injuries: First aid for fractures, sprains, strains, and dislocations.
- Medical Emergencies: Basic recognition and initial care for common medical issues like fainting, seizures, poisoning, bites, and stings.
- Secondary Survey and Ongoing Assessment: A more detailed check for injuries once immediate threats are managed.
- Record Keeping: Following relevant procedures for detailing the casualty’s condition and the techniques applied.
For specific local requirements and course details, you can refer to organizations like the Bangladesh Red Crescent Society which offers specific training based on local standards.
Study of OTC Drugs for RMP Course/Rural Medical Practitioner
OTC Drugs are important for RMP Course/Rural Medical Practitioner. A study of Over-The-Counter (OTC) drugs typically covers main topics related to prevalence of use, types of medications, reasons for self-medication, and associated knowledge, attitudes, and practices.
Here are the main topics typically included in a study of OTC drugs:
Demographics and Use Prevalence
- Prevalence of Self-Medication: The overall rate at which individuals use OTC drugs without a prescription.
- Socio-demographic Variables: How factors such as age, gender, education level, occupation (e.g., health science student status), and income influence OTC drug use.
- Frequency of Use: How often people take OTC medications (e.g., in the past three months, past year).
Types of OTC Drugs and Ailments
- Common Ailments/Conditions: The specific symptoms or minor illnesses for which people use OTC drugs:
- Fever and headache
- Cough, cold, and allergy symptoms
- Gastric issues (acidity, stomach pain, diarrhea, constipation)
- General/muscle pain
- Skin conditions
- Frequently Used Drug Classes: The types of medications used:
- Analgesics and Antipyretics (pain relievers and fever reducers, e.g., NSAIDs)
- Cough and cold preparations
- Antacids and H2 blockers
- Antihistamines
- Vitamins and nutritional supplements
- Note: Studies often also examine the misuse of prescription-only drugs like antibiotics when sold without a prescription.
Motivations and Information Sources
- Reasons for Use: The driving factors for choosing self-medication:
- Perception that the illness is minor
- Quick relief or convenience (lack of time to see a doctor)
- Prior experience with the drug
- Cost savings (avoiding consultation fees)
- Influence from peers, family, or advertising
- Sources of Information: Where users get information about the medications (e.g., reading material/labels, pharmacists, friends/family, old prescriptions, media).
Knowledge, Attitudes, and Practices (KAP)
- Knowledge Assessment: The level of understanding regarding:
- Proper dosage and directions
- Potential side effects, contraindications (e.g., during pregnancy or for children), and interactions with other drugs
- Awareness of the difference between OTC and prescription-only medications
- Proper storage and expiry dates
- Attitudes and Perceptions: Beliefs about the safety and efficacy of OTC drugs, and attitudes towards self-care.
- Practices: Specific behaviors related to use, such as:
- Reading the drug facts label
- Adhering to recommended dosages
- Actions taken in case of adverse effects
- Sharing medications with others
Regulatory and Public Health Implications
Recommendations: Strategies for improving public education, enforcing regulations, and promoting responsible self-medication practices among the general public and healthcare professionals.
Regulatory Framework: The legal status and control of OTC medicines in different regions (e.g., having a formal “OTC” category vs. a negative list of “prescription only” drugs).
Misuse, Abuse, and Adverse Effects: The extent of inappropriate use, potential for addiction (e.g., DXM or loperamide), and the resulting health consequences like delayed diagnosis, treatment failure, or organ damage.
Hematology for RMP Course/Rural Medical Practitioner
Hematology and Pathology cover blood cell formation, function, and diseases (like anemias, leukemias, lymphomas) and blood clotting (coagulation disorders), involving fundamental topics such as RBC/WBC/Platelet morphology, blood group serology, bone marrow exams, and blood banking, bridging general pathology (inflammation, cell injury) with systemic issues like hemostasis and malignancies. Key areas include RBC disorders (anemias, thalassemias, sickle cell), WBC disorders (leukemias, lymphomas), platelet/coagulation issues (bleeding/clotting), and diagnostic techniques like blood smears and bone marrow biopsies.
Core Areas of Study
- General Hematology (Benign): Red Blood Cell (RBC) & Hemoglobin Disorders, White Blood Cell (WBC) Disorders, Platelet Disorders, Hemostasis & Thrombosis.
- Malignant Hematology (Hemato-Oncology): Leukemias, Lymphomas, Myeloma, Myelodysplastic Syndromes (MDS).
- Immunohaematology: Blood Grouping & Transfusion Medicine.
Key Topics in Each Area
Red Blood Cell Disorders
- Anemias: Iron Deficiency, Megaloblastic (B12/Folate), Hemolytic (G6PD, Autoimmune), Aplastic Anemia.
- Hemoglobinopathies: Sickle Cell Disease, Thalassemia.
- Diagnostics: RBC Indices (MCV, MCH, MCHC), Reticulocyte Count, Peripheral Smear, Bone Marrow Examination, Osmotic Fragility.
White Blood Cell Disorders & Malignancies
- Disorders: Leukocytosis, Leukopenia, Infectious Mononucleosis.
- Malignancies: Acute Leukemias (ALL, AML), Chronic Leukemias (CML, CLL), Lymphomas (Hodgkin, Non-Hodgkin), Multiple Myeloma.
- Diagnostics: WBC Counts, Differential Counts, Bone Marrow Biopsy/Aspiration.
Platelets & Coagulation
- Disorders: Thrombocytopenia (ITP, TTP), DIC, Hemophilia A/B, Von Willebrand Disease.
- Mechanisms: Primary & Secondary Hemostasis, Coagulation Cascade, Anticoagulation.
- Diagnostics: Bleeding Time, Prothrombin Time (PT), Activated Partial Thromboplastin Time (aPTT).
General & Transfusion Pathology
- Blood Components: Composition of Blood, Plasma Proteins, Erythropoiesis.
- Immunity: Immune Mechanisms, Blood Groups (ABO/Rh), Transfusion Reactions, Coombs Test.
- Blood Banking: Cross-matching, Blood Component Therapy.
Foundational Concepts (Pathology Link)
- Cell Injury & Inflammation: Basics relevant to blood disorders.
- Hemodynamic Disorders: Edema, Thrombosis.
- Iron & Vitamin Metabolism: Key to RBC disorders.
Pathology for Medical Practice for RMP Course/Rural Medical Practitioner
The main topics for the subject of Pathology for Medical Practice are divided into two main areas: General Pathology (fundamental disease mechanisms) and Systemic Pathology (diseases affecting specific organ systems).
Key areas in Pathology for Medical Practice include General Pathology, covering fundamental disease mechanisms like cell injury, inflammation, and neoplasia, and Systemic Pathology, which applies these principles to specific organ systems. Systemic topics include conditions affecting the cardiovascular, respiratory, gastrointestinal, renal, hematologic, endocrine, and central nervous systems. The field also includes specialized diagnostic techniques like histopathology, cytopathology, clinical pathology, molecular pathology, and forensic pathology. For further details on these topics, refer to hrtdei.com blogs.hrtdei.com. A frequently recommended textbook for medical students is
Robbins & Cotran Pathologic Basis of Disease.
Human Microbiology for RMP Course/Rural Medical Practitioner
The main topics in human microbiology cover fundamental concepts of microbial life, their interactions with the human body, the body’s immune response, and practical applications in medicine and public health.
Key subject areas and their main topics include:
1. General Microbiology
This foundational area covers the basic science of microorganisms.
- Microbial Diversity and Classification: The study of different types of microorganisms, including bacteria, viruses, fungi, protozoa, and algae.
- Microbial Anatomy & Physiology: Structure and function of microbial cells (e.g., bacterial cell walls, flagella).
- Microbial Growth and Reproduction: Understanding how microorganisms multiply and the factors affecting their growth (e.g., bacterial growth curves, anaerobic culture methods).
- Microbial Genetics: How genetic information is stored, replicated, and transferred in microbes (e.g., horizontal gene transfer, plasmids, bacteriophages).
- Sterilization and Disinfection: Methods used to control microbial growth in healthcare and laboratory settings, including the use of autoclaves, disinfectants, and antiseptics.
2. Immunology
Immunology is essential to human microbiology, as it explores the body’s defense mechanisms against pathogens.
- Innate vs. Acquired Immunity: The differences between the body’s natural defenses and specific immune responses.
- Antigens and Antibodies: The role of antigens in triggering an immune response and the structure/function of antibodies (immunoglobulins).
- Immune System Components: The organs, cells, and soluble components (like the complement system and cytokines) involved in immunity.
- Hypersensitivity and Autoimmunity: Abnormal immune responses, including allergies and autoimmune disorders.
- Vaccines: Types and mechanisms of vaccines and immunization.
3. Medical Microbiology & Pathogenesis
This major specialization focuses on the microorganisms that cause human diseases and the mechanisms of infection.
- Bacteriology: Study of pathogenic bacteria, including their virulence factors, pathogenesis, clinical manifestations, and lab diagnosis (e.g., Staphylococcus, Streptococcus, Mycobacterium tuberculosis).
- Virology: Study of viruses, their isolation techniques, classification, and diseases (e.g., HIV, Hepatitis, Influenza).
- Mycology and Parasitology: Study of pathogenic fungi and parasites, their life cycles, and diagnosis of related infections (e.g., malaria, amoebiasis).
- Infection Control: Topics such as healthcare-associated infections (HAIs), hand washing protocols, and biomedical waste management.
- Antimicrobial Resistance (AMR): Mechanisms of resistance development and strategies for spread prevention.
4. Applied and Clinical Microbiology
This area bridges theoretical knowledge with practical applications in healthcare, industry, and the environment.
- Diagnostic Microbiology: Lab techniques like Gram staining, biochemical identification tests, and antimicrobial susceptibility testing used to identify infectious agents from patient samples.
- The Human Microbiome: Research into the complex communities of microbes that live in and on the human body and their influence on health and disease.
- Pharmaceutical Microbiology: Focuses on the use of microbes in drug development, quality control of pharmaceutical products, and the study of antibiotics.
Practice of Medicine for RMP Course/Rural Medical Practitioner
The practice of medicine encompasses a wide range of subjects, fundamentally divided into basic sciences, para-clinical subjects, and clinical subjects. The main topics within clinical medicine focus on the core skills and knowledge needed to diagnose, treat, and manage patients.
Core Clinical Practice Topics
The foundational skills required for practicing medicine include:
- History Taking: Gathering a detailed medical history from the patient.
- Physical Examination: Performing a thorough physical assessment of the patient’s body systems.
- Investigations: Ordering and interpreting laboratory tests and imaging studies.
- Diagnosis: Determining the nature of a disease or condition based on gathered information.
- Principles of Treatment: Developing and implementing a management plan, which may involve pharmaceuticals, surgery, or other therapies.
- Communication Skills: Effectively communicating with patients and their families, as well as other healthcare professionals.
- Doctor-Patient Relationship & Ethics: Maintaining professional relationships and adhering to ethical principles in patient care.
- Patient Safety: Ensuring the well-being and safety of patients throughout their care.
Major Medical Specialties and Sub-disciplines
Medical practice is further organized into various specialties, allowing doctors to focus on specific body systems, patient populations, or types of treatment:
Internal Medicine Subspecialties
Internal medicine deals with the prevention, diagnosis, and treatment of internal diseases. Sub-disciplines include:
- Cardiology (heart and blood vessels)
- Endocrinology (hormonal systems)
- Gastroenterology (digestive system)
- Geriatrics (elderly care)
- Hematology (blood)
- Infectious Disease
- Nephrology (kidneys)
- Oncology (cancer)
- Pulmonology (respiratory system)
- Rheumatology (musculoskeletal and autoimmune conditions)
Surgical Specialties
These specialties involve operative techniques to treat diseases and injuries:
- General Surgery
- Neurosurgery
- Orthopedic Surgery (musculoskeletal system)
- Ophthalmology (eyes)
- Otorhinolaryngology (ear, nose, and throat)
- Plastic Surgery
- Urology (urinary system)
- Trauma Surgery
Other Major Specialties
- Pediatrics (child health)
- Family Medicine/Primary Care (comprehensive healthcare for individuals and families)
- Emergency Medicine (acute care of injury and sudden illness)
- Psychiatry (mental health)
- Dermatology (skin)
- Radiology (medical imaging interpretation)
- Pathology (study of disease causes and mechanisms)
The practice of medicine bridges the gap between theoretical knowledge from basic sciences (anatomy, physiology, biochemistry) and practical, patient-centered care.
Cardiovascular Anatomy For RMP Course/Rural Medical Practitioner
The main topics in cardiovascular anatomy cover the structure and function of the heart, the network of blood vessels, and the principles of blood circulation.
I. The Heart
The heart is the muscular pump that drives blood circulation. Key anatomical topics include:
- Location and Structure: Position within the thoracic cavity (mediastinum), its size, and the protective pericardium.
- Heart Wall Layers: The endocardium (inner), myocardium (muscle middle layer), and epicardium (outer, also visceral pericardium).
- Chambers: The four chambers—right atrium, right ventricle, left atrium, and left ventricle—separated by the septum.
- Valves: The four valves (tricuspid, pulmonary, mitral, and aortic) that ensure unidirectional blood flow and prevent backflow.
- Coronary Circulation: The system of coronary arteries and veins that supplies the heart muscle tissue itself with oxygen and nutrients.
- Conduction System: The specialized electrical system, including the sinoatrial (SA) node (the heart’s natural pacemaker), which generates electrical impulses for rhythmic contraction.
II. Blood Vessels
This topic covers the extensive network of tubes that transport blood throughout the body.
- Types and Structure:
- Arteries: Carry oxygenated blood away from the heart (except for the pulmonary artery). They have thick, muscular, elastic walls to withstand high pressure.
- Veins: Carry deoxygenated blood back to the heart (except for the pulmonary veins). They have thinner walls and contain valves to prevent backflow against gravity.
- Capillaries: Tiny, thin-walled vessels that form networks within tissues for the exchange of oxygen, nutrients, and waste products.
- Major Vessels: The aorta (largest artery), superior and inferior vena cavae (major veins returning blood to the heart), and pulmonary arteries and veins.
III. Blood Circulation
This topic details the pathways and mechanics of blood flow.
- Pulmonary Circulation: The low-pressure circuit that transports deoxygenated blood from the right side of the heart to the lungs for oxygenation and returns oxygenated blood to the left atrium.
- Systemic Circulation: The high-pressure circuit that pumps oxygenated blood from the left side of the heart to the rest of the body’s tissues and organs, returning deoxygenated blood to the right atrium.
- The Cardiac Cycle: The sequence of events in a single heartbeat, including diastole (relaxation/filling) and systole (contraction/ejection of blood).
- Blood Composition & Function: The components of blood (plasma, red and white blood cells, platelets) and their role in transport and immunity.
Understanding these core anatomical components and their integrated functions is essential for grasping how the cardiovascular system maintains homeostasis in the body. For visual examples of these topics, you can explore detailed diagrams of the heart’s anatomy or the overall circulatory system.
Orthopedic Anatomy For RMP Course/Rural Medical Practitioner
The main topics in orthopedic anatomy center on the structure and function of the entire musculoskeletal system, including bones, joints, muscles, tendons, and ligaments. Key areas of study include:
General Principles & Basic Sciences
- Bone Structure and Function: Understanding the composition of compact and cancellous bone, as well as the structure of growth plates.
- Joints: The anatomy, function, and classification of different types of joints (e.g., synovial, cartilaginous), including ligaments and menisci.
- Muscles, Tendons, and Ligaments: The structure, function, and common disorders affecting these soft tissues.
- Neurovascular Structures: Anatomy of major nerves (ulnar, median, radial, sciatic) and blood vessels (axillary artery, saphenous vein), as their injury or entrapment often correlates with orthopedic conditions.
- Orthopaedic Terminology: Standardized language for describing injuries, conditions, and procedures.
Regional Orthopedic Anatomy
Orthopedic anatomy is often studied regionally to understand the specific complexities of each area:
- Spine: Cervical, thoracic, and lumbar spine anatomy, including vertebral columns, spinal cord, and common issues like disc prolapse and scoliosis.
- Upper Extremity: Shoulder, arm, elbow, forearm, wrist, and hand anatomy, including structures like the brachial plexus, carpal tunnel, and specific joints.
- Lower Extremity: Hip, thigh, knee, leg, ankle, and foot anatomy, including major joints and arches of the foot.
Pathology and Clinical Conditions
Anatomical knowledge is essential for understanding the diagnosis and treatment of specific conditions:
- Fractures and Dislocations: General principles, classification systems (e.g., Salter-Harris, Rang), management techniques, and common fracture sites (e.g., Colles’, supracondylar humerus).
- Sports Injuries: Focus on common traumatic disorders of joints, such as cruciate ligament and meniscal injuries.
- Infections and Tumors: Diseases of bones and joints, including osteomyelitis, septic arthritis, and the differentiation of benign and malignant bone tumors.
- Metabolic and Systemic Diseases: Conditions like osteoporosis, rickets, osteomalacia, Paget’s disease, gout, and osteoarthritis.
- Pediatric Orthopedics: Congenital disorders and conditions affecting the growing skeleton, such as clubfoot, congenital dislocation of the hip, and Perthes’ disease.
Surgery For RMP Course/Rural Medical Practitioner
Surgery as a subject covers broad areas like General Surgery (foundational for all specialties) and specific branches such as Cardiothoracic, Neurosurgery, Plastic Surgery, Pediatric Surgery, Orthopedics, & Oncology, focusing on diagnosis, surgical techniques (minimally invasive, robotic), patient safety, pre/post-op care, and core sciences like anatomy & physiology. Main topics involve managing diseases, injuries, congenital issues through cutting, repairing, or removing tissues, using advanced tools like endoscopes, lasers, and robots.
Core & Foundational Topics
- Anatomy & Physiology: The bedrock of all surgical knowledge.
- Pathology & Immunology: Understanding disease processes.
- Wound Management & Healing: Principles of closing and caring for surgical wounds.
- Shock & Resuscitation: Managing critical patient conditions.
- Patient Safety & Anesthesia: Essential for safe procedures, covering pain management and monitoring.
Major Surgical Specialties
- General Surgery: Broad scope, covering abdomen, breast, colorectal, etc..
- Cardiothoracic Surgery: Heart and lungs.
- Neurosurgery: Brain, spine, and peripheral nerves.
- Orthopedic Surgery: Bones, joints, ligaments, and trauma.
- Plastic & Reconstructive Surgery: Reshaping and repairing tissues.
- Pediatric Surgery: Surgery for infants, children, and adolescents.
- Oncology Surgery: Cancer treatment.
- Vascular Surgery: Blood vessels.
Key Surgical Techniques & Advances
- Minimally Invasive Surgery (MIS): Laparoscopy, endoscopy, robotics.
- Laser & Fiber Optics: Advanced tools for precision.
- Surgical Stapling & Hemostats: Techniques for tissue repair and bleeding control.
Other Important Areas
- Trauma Surgery: Emergency management of severe injuries.
- Organ Transplantation: Replacing diseased organs.
- Bioterrorism & Disaster Medicine: Surgical response to mass casualty events.
Generel Chemistry For RMP Course/Rural Medical Practitioner
General Chemistry covers fundamental concepts like Atomic Structure, Bonding, Periodic Trends, Stoichiometry, States of Matter (Gases, Liquids, Solids), Thermochemistry, Kinetics, Equilibrium, and Acid-Base Chemistry, forming the basis for understanding matter, energy, and their transformations, essential for medicine and other sciences. Key areas include understanding elements, compounds, reactions, solutions, and fundamental laws governing them, bridging physical and life sciences.
Core Topics in General Chemistry:
- Fundamentals of Matter:
- Atoms, Elements, Molecules, Ions, Compounds, Mixtures.
- Basic Atomic Structure (protons, neutrons, electrons, isotopes).
- Quantum Mechanics & Electron Configuration.
- Periodic Table & Periodic Trends (size, ionization energy).
- Chemical Bonding & Structure:
- Ionic & Covalent Bonding.
- Molecular Geometry & VSEPR Theory.
- Intermolecular Forces.
- Reactions & Stoichiometry:
- Chemical Equations & Balancing.
- Stoichiometry (mole ratios, limiting reactants).
- Redox Reactions & Oxidation Numbers.
- States of Matter:
- Gases (Gas Laws, Kinetic Molecular Theory).
- Liquids & Solids (Phase Changes, Properties).
- Thermochemistry & Kinetics:
- Energy, Heat, Work, & the Laws of Thermodynamics.
- Chemical Kinetics (reaction rates).
- Solutions & Equilibria:
- Solutions, Solutes, Solvents, & Colligative Properties.
- Chemical Equilibrium & Le Chatelier’s Principle.
- Acids, Bases, & pH (Acid-Base Chemistry).
- Electrochemistry & Nuclear:
- Electrochemistry (Redox in Cells).
- Nuclear Chemistry (basic concepts).
These topics build sequentially, from the smallest particles (atoms) to complex reactions and energy changes, providing a foundation for specialized chemistry fields like Organic, Inorganic, Physical, and Biochemistry.
Medical Biochemistry For RMP Course/Rural Medical Practitioner
Medical Biochemistry covers fundamental biomolecules (carbs, proteins, lipids, nucleic acids), metabolism (energy, pathways for all), enzymology, molecular biology (DNA, RNA, gene expression), cell biology, genetics, and integrated clinical aspects like hormones, nutrition, immunology, and disease mechanisms (e.g., diabetes, cancer). Key topics include Krebs cycle, electron transport chain, protein synthesis, bioenergetics, and specific disorders linked to metabolic errors or genetic defects, crucial for understanding health and disease.
Core Areas of Medical Biochemistry
- Biomolecules & Cell Biology:
- Structure & function of carbohydrates, lipids, proteins, nucleic acids.
- Cell structure, organelles, membranes, buffers, pH.
- Metabolism & Bioenergetics:
- Carbohydrate, Lipid, Amino Acid, Nucleic Acid metabolism.
- Energy production (Glycolysis, TCA cycle, ETC).
- Integration of metabolic pathways (e.g., gluconeogenesis, fatty acid oxidation).
- Molecular Biology & Genetics:
- DNA structure, replication, repair, gene expression (transcription, translation).
- Gene regulation, genetics, and genetic disorders.
- Enzymology:
- Enzyme kinetics, function, regulation, and clinical significance (marker enzymes).
- Clinical & Applied Biochemistry:
- Endocrinology: Hormones (structure, function, disorders).
- Nutrition: Vitamins, minerals, protein-energy malnutrition.
- Immunology: Immunoglobulins, immune responses.
- Pathology: Biochemical basis of diseases (diabetes, cancer, atherosclerosis, liver/kidney function).
- Pharmacology: Drug metabolism, interactions.
- Tools & Techniques:
- Laboratory techniques, diagnostics (LFTs, KFTs), biomarkers, and research methods.
Why It Matters
Medical Biochemistry connects basic science to clinical medicine, explaining how body chemistry relates to health, disease (pathology), drug action (pharmacology), and nutritional needs, making it vital for diagnostics and treatment.
Medical Diagnosis For RMP Course/Rural Medical Practitioner
The term “medical diagnosis subject” generally refers to the specific branches of medicine or categories of conditions that are the focus of diagnostic study and practice. These can be categorized by body system, disease type, or the diagnostic methodology used.
Main topics and subjects related to medical diagnosis include:
By Body System/Specialty
- Cardiology: Diagnosis of heart and blood vessel disorders, such as coronary artery disease and heart failure.
- Pulmonology: Diagnosis of respiratory diseases, including asthma, pneumonia, and pulmonary disorders.
- Gastroenterology: Diagnosis of disorders affecting the esophagus, stomach, intestines, liver, biliary tract, and pancreas.
- Neurology: Diagnosis of nervous system disorders, such as Alzheimer’s disease or multiple sclerosis.
- Dermatology: Diagnosis of diseases of the skin, hair, and nails.
- Endocrinology: Diagnosis of endocrine disorders, including diabetes mellitus and thyroid conditions.
- Oncology: Diagnosis and staging of cancers, often using histopathological diagnosis (microscopic tissue examination).
By Disease Category
- Infectious Diseases: Diagnosis of conditions caused by bacteria, viruses, fungi, or parasites, such as malaria, HIV, or acute diarrheal disorders.
- Immunology and Rheumatology: Diagnosis of autoimmune and allergic disorders.
- Hematology: Diagnosis of blood disorders like anemia, leukemia, and bleeding disorders.
- Psychiatry: Diagnosis of psychiatric disorders and mental health conditions.
By Diagnostic Methodology
- Medical Imaging: The use of technologies like X-rays, CT scans, and MRIs to diagnose conditions.
- Clinical Pathology: The use of laboratory tests on blood (e.g., blood chemistry, complete blood count), urine, and other body fluids for diagnosis.
- Genetics: The study and diagnosis of genetic diseases and inherited conditions.
For comprehensive information on the diagnostic process for a wide range of conditions, resources like Current Medical Diagnosis & Treatment provide detailed coverage of all major medical fields
Common Cardiovascular Problems For RMP Course/Rural Medical Practitioner
Common Cardiovascular Problems are Hypertension, Hypotension, Postural Hypotension, Tachycardia, Bradycardia, Abnormal Pulse, Deficiency of Shechurated Oxygen, Abnormal Heart Sound, Increase Bad Cholesterol, Heart Failure, Edema, etc. These problems are discussed as elaborately as possible.
সাধারণ কার্ডিওভাসকুলার সমস্যাগুলি হল উচ্চ রক্তচাপ, হাইপোটেনশন, পোস্টুরাল হাইপোটেনশন, টাকাইকার্ডিয়া, ব্র্যাডিকার্ডিয়া, অস্বাভাবিক পালস, শেচুরেটেড অক্সিজেনের ঘাটতি, অস্বাভাবিক হার্টের শব্দ, খারাপ কোলেস্টেরল বৃদ্ধি, হার্ট ফেইলিওর, শোথ ইত্যাদি। এই সমস্যাগুলি যতটা সম্ভব বিশদভাবে আলোচনা করা হয়েছে।
Common cardiovascular problems are a major public health concern globally. Key topics often revolve around the most prevalent conditions, their underlying causes, and management strategies.
Main topics for common cardiovascular problems include:
- Coronary Artery Disease (CAD)/Coronary Heart Disease (CHD): This is one of the most common and significant cardiovascular diseases, primarily caused by atherosclerosis (plaque buildup) in the heart’s arteries. This can lead to angina (chest pain), heart attacks (myocardial infarction), and heart failure.
- Hypertension (High Blood Pressure): A very common condition and a major risk factor for the development of many other cardiovascular diseases, including CAD, heart failure, and stroke.
- Heart Failure: A complex condition where the heart cannot pump blood efficiently enough to meet the body’s needs. It often occurs as a final stage of most other cardiovascular diseases.
- Cerebrovascular Disease (Stroke): This involves the blood vessels supplying the brain. Impaired blood flow can lead to a stroke or transient ischemic attacks (TIAs).
- Arrhythmias: Problems with the heart’s rhythm or conduction system. Atrial fibrillation is the most common sustained cardiac arrhythmia.
- Peripheral Artery Disease (PAD): This involves arterial disease predominantly affecting the limbs, which can result in pain and cramping (claudication).
- Valvular Heart Disease: Conditions affecting the heart valves (aortic, mitral, pulmonary, and tricuspid), which regulate blood flow within the heart.
- Aortic Aneurysms: Weakening and bulging of the aorta, often due to atherosclerosis, which can occur in the thoracic or abdominal areas.
- Congenital Heart Disease: Heart defects present at birth, representing the most prevalent congenital condition globally.
These topics also encompass important related subjects such as preventive cardiology (lifestyle modifications and risk factor control like diet, exercise, and smoking cessation) and imaging techniques used for diagnosis.
Common Pediatric Problems & Proper Management for RMP Course/Rural Medical Practitioner
Common Pediatric Problems: Pediatric Respiratory Problems, Pediatric Digestive Problems, Pediatric Skin Problems. These are discussed in the Rural Medical Practitioner Course. Pediatric Respiratory Problems are Pediatric Pneumonia, Pediatric Rhinitis, Pediatric Asthma, etc. Pediatric Digestive Problems are Rotavial Diarrhea, Pediatric Flatulence, Pediatric Abdominal Discomfort, Pediatric Vomiting, and Pediatric Constipation. Pediatric skin problems are tineasis and oral Candidiasis, and they are especially common in tinea capitis and tinea crusis.
Primary Gastrology for Long RMP Course/Rural Medical Practitioner
Gastrology for RMP is an important subject. This Subject discusses the important part of Gastrointestinal Anatomy, Gastrointestinal Drugs, and Medicines, and Gastrointestinal Diseases as elaborately as possible. Common Points of Gastrointestinal Anatomy and Physiology are Anatomy of Tongue, Anatomy or Oral Cavity, Anatomy of the Esophagus, Physiology of Tongue, Physiology of Evola, Physiology of Epiglotis, Anatomy of Stomach, Anatomy of Small Intestine, Anatomy of Large Intestine, Anatomy of Cecum and Appendix, Physiology of Appendix, Digestive Sphincters, etc. Common Gastrointestinal Drugs are Anti Vomiting Drugs, Anti Ulcer Drugs, Motility Drugs, Antimotility Drugs, Laxative Drugs, Anti Diarrheal Drugs, Some Antimicrobial Drugs for Gastrointestinal Infectious Diseases.
আরএমপির জন্য গ্যাস্ট্রোলজি একটি গুরুত্বপূর্ণ বিষয়। এই বিষয়টি গ্যাস্ট্রোইনটেস্টাইনাল অ্যানাটমি, গ্যাস্ট্রোইনটেস্টাইনাল ড্রাগস, এবং মেডিসিনস এবং গ্যাস্ট্রোইনটেস্টাইনাল রোগের গুরুত্বপূর্ণ অংশ যতটা সম্ভব বিশদভাবে আলোচনা করে। গ্যাস্ট্রোইনটেস্টাইনাল অ্যানাটমি এবং ফিজিওলজির সাধারণ পয়েন্টগুলি হল জিহ্বার অ্যানাটমি, অ্যানাটমি বা ওরাল ক্যাভিটি, খাদ্যনালীর অ্যানাটমি, জিহ্বার শারীরবৃত্তবিদ্যা, ইভোলার শারীরবৃত্তি, এপিগ্লোটিসের শারীরবৃত্তি, পেটের অ্যানাটমি, অ্যানাটমি অফ স্মল ইনস্টেস্টিন, অ্যানাটমি অফ দ্য অ্যানাটমি। সিকাম এবং অ্যাপেন্ডিক্স, অ্যাপেন্ডিক্সের ফিজিওলজি, ডাইজেস্টিভ স্ফিন্টার, ইত্যাদি। সাধারণ গ্যাস্ট্রোইনটেস্টাইনাল ওষুধগুলি হল বমি প্রতিরোধক ওষুধ, অ্যান্টি আলসার ড্রাগস, গতিশীলতা ওষুধ, অ্যান্টিমোটিলিটি ড্রাগস, ল্যাক্সেটিভ ড্রাগস, অ্যান্টি ডায়রিয়াল ড্রাগস, কিছু অ্যান্টিমাইক্রোবিয়াল ড্রাগস যা গ্যাস্ট্রোইনফেক্টের জন্য।
Practicle Class For RMP Course/Rural Medical Practitioner
Heart Beat, Heart Rate, Heart Sound, Pulse, Blood Pressure, Hypertension, Hypotension, First Aid Box, Auscultation, Inhaler, Rota Haler, nebulizer, Diabetes, Injection I/B-I/M, Cleaning, Dressing, Bandaging, saline, CPR, Stitching, Body Temperature, Blood Grouping, Blood Grouping, Nasal Tube gel, Hand Wash, Cyanosis, Dehydration Test, Edema Test.
Heart Beat & Heart Rate Class for RMP Course/Rural Medical Practitioner
A practical class for measuring heartbeat and heart rate typically involves learning to take a pulse, conducting experiments to measure heart rate during different activities, and analyzing the results.
Part 1: Learning to Measure Your Pulse
The pulse is the physical manifestation of the heart pumping blood through your arteries and is a direct measure of your heart rate (beats per minute, or bpm).
Location of Pulse:
- Wrist (radial artery): Place the tips of your first two fingers on the palm side of the partner’s wrist, below the thumb. Press firmly until you feel the pulse.
- Neck (carotid artery): Find the soft area on either side of the windpipe. Note: Use caution and light pressure when using the carotid artery site, as excessive pressure can slow the heart rate.
Measurement Technique:
- Using a timer or stopwatch, count the number of beats you feel in a specific amount of time.
- Count for 30 seconds and multiply by 2 to get the beats per minute (bpm).
- Alternatively, count for 15 seconds and multiply by 4. For a quicker measure, count for 6 seconds and multiply by 10.
Part 2: Experimenting with Activity Levels
The primary activity involves measuring how physical exertion affects heart rate. Students will measure their heart rate at rest, during exercise, and during recovery.
Materials Needed:
- Timer/Stopwatch
- Pen and paper for recording data
- Worksheet/Table
Procedure:
- Resting Heart Rate: Sit quietly for 3-5 minutes. Measure and record your pulse rate. A normal resting heart rate for adults is 60 to 100 bpm.
- Physical Activity: Perform a specific exercise for a set period (e.g., 100 jumping jacks, running in place for 2 minutes).
- Immediately After Activity: Immediately after stopping the exercise, measure and record your heart rate. It should be significantly higher than your resting rate.
- Recovery Heart Rate: Measure your heart rate again after a few minutes (e.g., 2 minutes and 4 minutes post-exercise) to observe how quickly it returns to normal.
Part 3: Analysis and Discussion
After collecting data, students can analyze and discuss their findings.
- Graphing Results: Plot the heart rate data at different stages (rest, immediately after exercise, during recovery) to visually represent the effect of physical activity.
- Discussion Points:
- Why does heart rate increase during exercise? (The heart pumps faster to move oxygenated blood more quickly to muscles).
- How quickly does the heart rate return to resting levels? This is a measure of physical fitness.
- How did predictions compare to actual results?.
For additional resources and ideas, the Irish Heart Foundation and BioEd Online offer detailed lesson plans.
Blood Pressure Class for RMP Course/Rural Medical Practitioner
A practical class for blood pressure involves learning to use a sphygmomanometer and stethoscope to measure blood pressure (BP), understanding patient positioning, finding the brachial artery, estimating systolic/diastolic pressures by listening for Korotkoff sounds (first sound for systolic, cessation for diastolic), and interpreting readings using standard guidelines (e.g., <120/80 mmHg is normal). Key steps include preparing the patient, applying the cuff correctly, inflating and deflating the cuff at a steady rate (2-3 mmHg/sec), documenting results, and practicing with digital devices too.
Key Components of a Practical Session
- Equipment: Learn to use manual (aneroid/mercury) and digital sphygmomanometers with a stethoscope.
- Patient Prep: Ensure the patient is rested (5 mins), back supported, feet flat, arm at heart level, and bladder empty; avoid caffeine/tobacco for 30 mins prior.
- Cuff Placement: Apply cuff to bare skin, 2 inches above elbow bend, align arrow with brachial artery.
- Procedure (Auscultation):
- Estimate Systolic: Palpate brachial artery, inflate cuff until pulse disappears (this is estimated systolic).
- Auscultate: Place stethoscope over artery, inflate cuff 30 mmHg above estimated systolic.
- Deflate Slowly: Open valve to drop pressure 2-3 mmHg/sec.
- Listen for Sounds: First sound = Systolic; Sound stops = Diastolic (or last sound, depending on guidelines).
- Documentation: Record the reading (e.g., 110/70 mmHg) and the arm used, noting if rounded to nearest even number.
- Practice & Interpretation: Repeat readings, check against guidelines (e.g., <120/80 mmHg is normal), and learn when to seek medical advice (e.g., persistent high readings or hypertensive crisis symptoms).
Resources for Practice
- YouTube Videos: Search for “How to take blood pressure manual” or “Korotkoff sounds practice” (e.g., by LevelUp RN, for clinical skills).
- Online Courses: PAHO offers courses on Home Blood Pressure Monitoring for patients and providers.
Hypertension & Hypotension Class for RMP Course/Rural Medical Practitioner
A practical class on hypertension and hypotension would focus on understanding blood pressure (BP) values, diagnosis methods, lifestyle management, and the different classes of medications used for treatment.
Core Concepts
- Normal Blood Pressure: Generally considered between 90/60 mm Hg and 120/80 mm Hg.
- Hypertension (High BP): Consistently elevated blood pressure, typically defined as a reading of 140/90 mm Hg or higher in a clinical setting (definitions may vary slightly by guideline).
- Hypotension (Low BP): Blood pressure below 90/60 mm Hg, which is often asymptomatic but can cause symptoms like dizziness or fainting.
- Orthostatic Hypotension: A specific type of low blood pressure that happens when moving from sitting or lying down to a standing position.
Practical Class Activities
A practical class could incorporate the following components:
- Blood Pressure Measurement: Hands-on training using a sphygmomanometer and stethoscope, or automated devices, to accurately measure BP in supine, sitting, and standing positions (especially relevant for diagnosing orthostatic hypotension).
- Case Studies: Analyzing hypothetical patient scenarios involving different stages of hypertension (Stage 1, 2, 3) or symptomatic hypotension to practice diagnosis and treatment planning.
- Lifestyle Interventions: Discussion and role-playing on counseling patients about non-pharmacological management strategies:
- Healthy diet (e.g., DASH diet).
- Regular physical activity.
- Weight management and limiting alcohol.
- Counter-maneuvers for orthostatic hypotension, such as standing up slowly and muscle tensing.
- Pharmacology Review: Understanding the mechanisms of action, side effects, and appropriate use of different classes of antihypertensive and pro-hypertensive medications:
- Antihypertensive classes: Diuretics, ACE inhibitors, Angiotensin II Receptor Blockers (ARBs), Calcium Channel Blockers, and Beta-blockers.
- Hypotension drugs: Midodrine, droxidopa, and rapid fluid infusion for acute cases.
- Patient Education Simulation: Practicing how to educate patients on home blood pressure monitoring (HBPM) protocols and the importance of adherence to treatment plans.
Resources for Further Learning
Educational materials and guidelines are available from authoritative sources:
- The American Heart Association and the European Society of Cardiology provide comprehensive guidelines on managing hypertension.
- The National Institutes of Health provides detailed information on both hypertension and hypotension.
What is the meaning of RMP?
RMP stands for RMP Course/Rural Medical Practitioner. This is a kind of Village Doctor Course. Durations of RMP Course/Rural Medical Practitioner are 6 Months, 1 Year, and 2 Years. The more you study the more you learn and the more you provide services. আরএমপি মানে হল রুরাল মেডিকেল প্র্যাকটিশনার। এটি এক ধরনের ভিলেজ ডক্টর কোর্স। আরএমপি কোর্সের সময়কাল 6 মাস, 1 বছর এবং 2 বছর। আপনি যত বেশি অধ্যয়ন করবেন তত বেশি শিখবেন এবং তত বেশি পরিষেবা প্রদান করবেন।
RMP Course/Rural Medical Practitioner Online
RMP Course/Rural Medical Practitioner Course Online. Mobile Phone No. 01797522136, 01987073965. You can study RMP Course/Rural Medical Practitioner Online from any part of the country and any part of the world. Weekly class 3 hours. Friday, Saturday, and Monday for Regular students. For job holders 3 hours weekly class in a day. 6 Months Course fee tk 26500/-, admission fee tk 10500/-, and monthly fee tk 2500/-. 1 year course fee tk 52500/-, admission fee tk 10500/-, monthly fee tk 3000/-, exam fee tk 3000/ semester. Theory classes through onlie and practical classes through offline. Practical classes will be held when you will come to our institute.
আরএমপি কোর্স অনলাইন। মোবাইল ফোন নং 01797522136, 01987073965। আপনি দেশের যেকোনো প্রান্ত থেকে এবং বিশ্বের যেকোনো প্রান্ত থেকে অনলাইনে আরএমপি কোর্স পড়তে পারেন। সাপ্তাহিক ক্লাস 3 ঘন্টা। নিয়মিত শিক্ষার্থীদের জন্য শুক্র, শনিবার এবং সোমবার। চাকরিজীবীদের জন্য দিনে ৩ ঘণ্টা সাপ্তাহিক ক্লাস। 6 মাসের কোর্স ফি টাকা 26500/-, ভর্তি ফি টাকা 10500/-, এবং মাসিক ফি 2500/- টাকা। 1 বছরের কোর্স ফি টাকা 52500/-, ভর্তি ফি টাকা 10500/-, মাসিক ফি টাকা 3000/-, পরীক্ষার ফি 3000/- সেমিস্টার। অনলাইনের মাধ্যমে থিওরি ক্লাস এবং অফলাইনের মাধ্যমে ব্যবহারিক ক্লাস। আপনি যখন আমাদের ইনস্টিটিউটে আসবেন তখন ব্যবহারিক ক্লাস অনুষ্ঠিত হবে।
RMP Course/Rural Medical Practitioner is a Village Doctor Course
RMP is a traditional village doctor course. It is being running from hundreds of years in Bangladesh. Still now there are many RMP doctors in Bangladesh. They are providing primary medical treatment in the rural area of our country. আরএমপি একটি ঐতিহ্যবাহী গ্রাম্য ডাক্তার কোর্স। বাংলাদেশে শত শত বছর থেকে এটি চলে আসছে। এখনো বাংলাদেশে অনেক RMP ডাক্তার আছে। তারা আমাদের দেশের গ্রামীণ এলাকায় প্রাথমিক চিকিৎসা প্রদান করছে।
Primary Midwifery for RMP Course/Rural Medical Practitioner Long Course
Primary Midwifery is an important subject for Female RMP Long Course. Female students can study and impliment Primary Midwifery for Rural Poor Female Patients at the time of child delivery. Many poor patients can not go to the hospital for the crises of money at the time of child delivery. Well trained female students can help the poor patient for normal delivery.
প্রাথমিক মিডওয়াইফারি মহিলা আরএমপি দীর্ঘ কোর্সের জন্য একটি গুরুত্বপূর্ণ বিষয়। মহিলা শিক্ষার্থীরা শিশু প্রসবের সময় গ্রামীণ দরিদ্র মহিলা রোগীদের জন্য প্রাথমিক মিডওয়াইফারি অধ্যয়ন করতে এবং অনুপ্রাণিত করতে পারে। সন্তান প্রসবের সময় টাকার সংকটে অনেক দরিদ্র রোগী হাসপাতালে যেতে পারেন না। ভাল প্রশিক্ষিত মহিলা শিক্ষার্থীরা স্বাভাবিক প্রসবের জন্য দরিদ্র রোগীকে সাহায্য করতে পারে।
Other Village Doctor Courses & Diploma Medical Courses
Other Village Doctor Courses are the LMAF Course, LMA Course, DMA Course, DMS Course, Paramedical Course, DPM Course, and DMDS Course. All these courses are available at HRTD Medical Institute.
 HRTD Medical Institute
HRTD Medical Institute





