Skin Specialty Training Course Details
Skin Specialty Training Course. Mobile No. 01987-073965, 01797-522136. PDT Skin VD 6 Months, PDT Skin VD 1 Year, PDT Skin VD 2 Years, PGT Skin VD 6 Months, PGT Skin VD 1 Year.

Skin VD means Skin and Venereal Disease. Venereal Diseases are those that affect the sexual organs of the reproductive system.

Course Fee for Skin Specialty Training Courses (PDT Skin VD) in Dhaka, Bangladesh
Skin Specialty Training Courses are PDT Skin VD Courses and PDT Dermatology Courses. Mobile No. 01987-073965, 01797-522136. PDT Skin VD 6 Months Tk 35000/-, PDT Skin VD 1 Year Tk 65000/-, PDT Skin VD 2 Years Tk 125000/-. https://studio.youtube.com/video/Z7WXMZpl0-E/edit
Course Fee for PGT Skin VD in Dhaka, Bangladesh
PGT Skin VD Course Fee. Mobile No. 01987-073965, 01797-522136. PGT Skin VD 6 Month Tk 60000/-, and PGT Skin VD 1 Year Tk 110000/-.
Location of Skin Specialty Training Center in Dhaka, Bangladesh
Location of Skin Specialty Training Center. Mobile No. 01987-073965, 01797-522136. HRTD Medical Institute, Abdul Ali Madbor Mansion, Section-6, Block-Kha, Road-1, Plot-11, Mirpur-10 Golchattar, Dhaka-1216.
Qualification for Admission to Skin Specialty Training Courses (PDT Skin VD Training Course)
Qualification for PDT Skin VD Course. Mobile No. 01987-073965, 01797-522136. 4 Years Medical Diploma/ Short Medical Diploma with Science Graduate.
Qualification for Admission to PGT Skin VD Training Course
Qualification for PGT Skin VD Course. Mobile No. 01987-073965, 01797-522136. MBBS from any Medical College.
Subjects for Skin Specialty Training Courses
Subjects for Skin Specialty Training Courses: Common Subjects for Skin VD Or Dermatology Specialty Courses are 1. Skin Anatomy & Physiology, 2. Fungal Infections, 3. Common Skin Problems, 4. Infectious Skin Diseases, 5. Reproductive Anatomy & Physiology, 6. Venereal Diseases, 7. Sexually Transmitted Diseases, 8. Pigmentation, 9. Allergic Dermatitis & Eczema, 10. Vitiligo, 11. Skin Malignancy, 12. Dermatological Drugs & Medicine, 13. Application of Dermatological Medicines, 14. Diabetic Foot & Skin Conditions, 15. Common Skin Rashes, 16. Steroids & Other Topical Skin Medicines.
Abscess & Boil Definition
Accumulation of pus in a tissue or organ in the body is called abscess. The accumulation of pus in the skin is called boil. Boil is an abscess that occurs in the skin. The causative organism for boil is Staphylococcus bacteria. These bacteria enter the body through tiny nicks or cuts in the skin or can travel down the hair to the follicle.
Cellulitis Definition and Causes
Inflammation of the subcutaneous connective tissue is called cellulitis. The inner layer of skin is called hypodermis of subcutaneous tissue. The components of hypodermis are fat and connective tissue. The causative organisms are Streptococcus and Staphylococcus.

Gonorrhoea Definition, Causes, and Clinical Feature
Infection with Neisseria gonorrhea is called gonorrhea. Neisseria gonorrhea usually infects the sexual organs. Clinical features for the male patient: Discharge through the urethra, Testitis, and Burning when urinating. Clinical features for the female patient: Discharge through the urethra, vulvitis, and Burning when urinating.
Carbuncle Definition and Causes
A Carbuncle is a cluster of boils caused by bacterial infection, most commonly with staphylococcus aureus or streptococcus pyogenes.
Syphilis Definition, Causes, and Clinical Feature
Syphilis is a Sexually Transmitted Disease Caused by the Spirochaetes named Treponema pallidum. There are three stages of Clinical features: 1st stage, 2nd stage, and 3rd stage. Clinical features in 1st stage: Small painless pink color open shore ( called a chancre) in sexual organs, painless ulcer, and then swelling of regional lymph nodes. Clinical feature in 2nd stage: Ulcer in Sexual organs, mouth, pharynx, and larynx. Excessive swelling of regional lymph nodes. Maculopapular rash on the palm of the hand and foot. Clinical features in 3rd stage: Cardiac problem, Neurogenic problem.
Vitiligo Definition, Causes and treatment
Loss of pigment in the skin due to destruction of color giving cells of skin by autoimmune disorders. Treatment of Vitiligo are Re pigmentation therapy, Camouflage Therapy, Light Therapy and Surgery.

Drugs Used in Skin Specialty Course and PDT Dermatology
Drugs used in Skin Specialty Course are Antibiotic Drugs, Antifungal Drugs, Anti Viral Drugs, Steroid Drugs, NSAID Drugs, Antihistamine Drugs, Anti Scabies Drugs, Burn Cream, Retinoid, Azelaic Acid, Salicylic Acid, Anti Leprosy Drugs, Liquid Nitrogen, Brimonidine, Epinephrine, Emollients, Hydroxychloroquine, Medicated Shampoos, and Hydroquinone.
Dermatology uses a wide range of drugs, including topical & oral steroids, antibiotics (like tetracyclines, clindamycin), retinoids (tretinoin, adapalene), antifungals, antivirals (acyclovir), and immunomodulators (pimecrolimus), plus newer systemic agents like JAK inhibitors and biologics for conditions like psoriasis and eczema, alongside drugs for other issues like minoxidil for hair loss or antihistamines for itching, targeting inflammation, infection, and cell growth.
Topical Treatments (Applied to Skin)
- Corticosteroids: Reduce inflammation (e.g., alclometasone, hydrocortisone).
- Retinoids (Vitamin A Derivatives): For acne and anti-aging (e.g., tretinoin, adapalene).
- Antibiotics: For bacterial infections (e.g., clindamycin, mupirocin).
- Antifungals: For fungal infections (e.g., butenafine).
- Antiparasitics: For mites/lice (e.g., crotamiton).
- Calcineurin Inhibitors: For eczema (e.g., pimecrolimus).
- Keratolytics: Like salicylic acid for acne/warts.
- Hydroquinone: For skin lightening/melasma.
Systemic Treatments (Oral/Injected)
- Antibiotics: Tetracyclines, dicloxacillin for acne, infections.
- Isotretinoin: Powerful oral retinoid for severe acne.
- Immunosuppressants: Methotrexate, cyclosporine, apremilast (PDE4 inhibitor) for psoriasis, eczema.
- Biologics: Targeted antibodies (e.g., TNF-alpha inhibitors, IL-12/23 inhibitors) for severe inflammatory conditions.
- Antivirals: Acyclovir, famciclovir for herpes viruses.
- Antihistamines: For itching (e.g., cetirizine, loratadine, fexofenadine).
- Minoxidil: For hair loss.
- Psychotropics: Tricyclic antidepressants (amitriptyline) for chronic itch/pain.
Key Drug Classes
- Anti-Inflammatories: Steroids, calcineurin inhibitors, JAK inhibitors.
- Anti-Infectives: Antibiotics, antifungals, antivirals, antiparasitics.
- Cell Growth Modulators: Retinoids, acitretin (for psoriasis).
- Immunomodulators: Biologics, immunosuppressants.
Dermatologists select drugs based on the condition (acne, psoriasis, eczema, infection, etc.), severity, and patient factors, often combining treatments for best results
Skin Anatomy & Physiology For Skin Specialty Course”
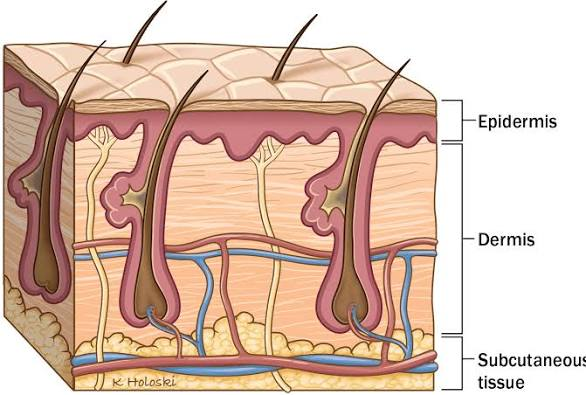
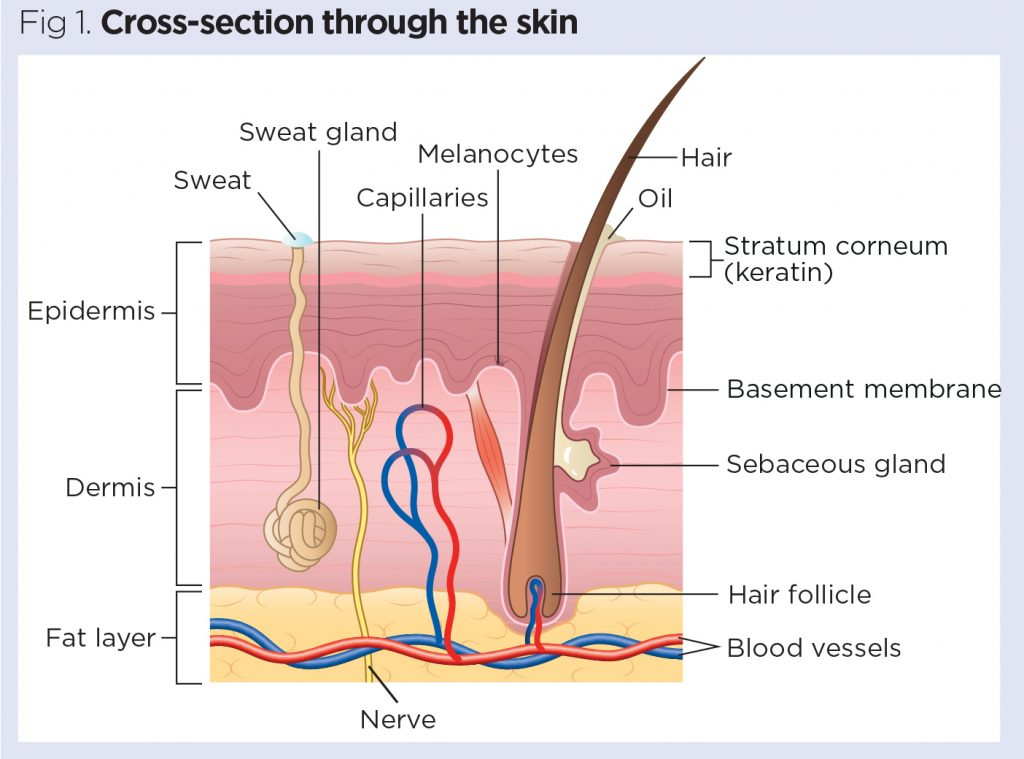
The skin is the body’s largest organ and is comprised of two main layers: the epidermis (outer) and the dermis (inner), which lie atop the subcutaneous tissue (hypodermis). Together with accessory structures like hair, nails, and glands, they form the integumentary system, which serves vital protective, regulatory, and sensory functions.
Anatomy of the Skin
The skin has three primary layers, each with distinct components and sublayers.
- Epidermis: The outermost, avascular layer of skin you can see and touch. It is primarily composed of keratinocytes and provides a waterproof barrier. It contains melanocytes (for pigment), Langerhans cells (for immunity), and Merkel cells (for touch sensation). The epidermis is further divided into five sublayers (strata) in thick skin (palms and soles) and four in thin skin:
- Stratum corneum: Outermost layer of dead, flat, keratin-filled cells that are constantly shed.
- Stratum lucidum: A thin, clear layer present only in thick skin.
- Stratum granulosum: Cells begin to die and produce keratin.
- Stratum spinosum: Cells have spiny projections and some cell division occurs.
- Stratum basale: The deepest layer, where new skin cells are continuously formed via mitosis and pushed upward.
- Dermis: Located beneath the epidermis, this thick layer contains connective tissue, collagen, and elastin fibers that provide strength and flexibility. It houses hair follicles, sebaceous (oil) glands, sweat glands, blood vessels, lymphatic vessels, and nerve endings. The dermis is divided into the papillary layer and the reticular layer.
- Subcutaneous Tissue (Hypodermis): While not technically a skin layer, it lies beneath the dermis and connects the skin to underlying muscles and bones. It is composed of loose connective tissue and adipose (fat) tissue, which provides insulation, cushioning, and an energy store.
Physiology and Functions of the Skin
The skin is a complex, multifunctional organ that is essential for survival. Key functions include:
- Protection: It serves as a primary physical, chemical, and biological barrier against pathogens, UV radiation, dehydration, and mechanical injury.
- Sensation: Nerve endings and specialized receptors in the dermis enable the perception of touch, pressure, vibration, pain, and temperature changes in the environment.
- Temperature Regulation: The skin regulates body temperature through sweating (evaporation cools the body) and by adjusting blood flow via vasodilation (heat release) and vasoconstriction (heat retention).
- Vitamin D Synthesis: Upon exposure to sunlight, the skin initiates the synthesis of vitamin D, which is crucial for calcium absorption and healthy bones.
- Excretion and Absorption: The skin aids in the minor excretion of waste products like urea through sweat and can absorb certain substances, such as topical medications.
- Immunity: Specialized immune cells (Langerhans cells) in the epidermis help the body fight off germs and infections.
Fungal infections For Skin Specialty Course
Fungal infections (mycosis) are diseases caused by a fungus that can affect the skin, nails, hair, or internal organs. Most common are superficial infections, which are treatable with antifungal medications, while deep (systemic) infections can be more serious, especially for individuals with weakened immune systems.
Common Types of Fungal Infections
Fungal infections are generally categorized by the body part they affect:
- Ringworm (Tinea): A highly contagious, common infection that causes a red, circular, scaly rash. The name changes based on location:
- Athlete’s foot (Tinea pedis): Affects the feet, especially between the toes, causing itching, peeling, and cracking.
- Jock itch (Tinea cruris): Causes an itchy, red rash in the groin and inner thighs.
- Scalp ringworm (Tinea capitis): Affects the scalp and can cause hair loss, primarily in children.
- Yeast Infections (Candidiasis): Caused by an overgrowth of the Candida yeast, which naturally lives on the body.
- Vaginal yeast infections: Common in women, causing itching, soreness, and unusual discharge.
- Oral thrush: Causes white patches in the mouth and throat, along with pain when eating or swallowing.
- Nail Infections (Onychomycosis): Makes fingernails or toenails thick, discolored (yellow, white, or brown), and brittle.
- Tinea versicolor: Causes discolored patches on the skin, often on the chest, back, and upper arms.
Symptoms
Symptoms vary depending on the type and location of the infection:
| Type of Infection | Common Symptoms |
|---|---|
| Superficial (Skin, Nails) | Itching, redness, rash, scaly or flaky skin, discolored/thick nails, white patches (mouth/throat). |
| Systemic (Lungs, Organs) | Fever, fatigue, cough, shortness of breath, muscle/joint pain, headaches, night sweats. |
Causes and Risk Factors
Fungi thrive in warm, moist environments. Common causes and risk factors include:
- A weakened immune system (due to conditions like HIV/AIDS, cancer, or immunosuppressant medications).
- Wearing tight, non-breathable clothing or footwear.
- Poor hygiene, such as not drying the skin thoroughly after showering.
- Walking barefoot in public areas (showers, locker rooms, pools).
- Sharing personal items like towels, clothing, or nail clippers.
- Taking antibiotics, which can kill beneficial bacteria that keep fungi in check.
Treatment and Prevention
Fungal infections are treated with antifungal medications. Mild skin infections often respond to over-the-counter creams, lotions, or powders, while more severe or systemic infections may require prescription-strength oral or intravenous medication.
Prevention primarily involves good hygiene and environmental awareness:
- Keep skin clean and dry, especially in skin folds and between toes.
- Wear clean, dry, and breathable clothing (like cotton underwear and socks).
- Avoid walking barefoot in public damp areas like showers or locker rooms.
- Do not share personal items (towels, clothing, etc.).
Common Skin Problems For Skin Specialty Course
Common skin problems range from temporary irritations to chronic conditions, caused by factors including genetics, infections, allergies, and environmental triggers. The most frequent issues include acne, eczema, and psoriasis, all of which have various treatment and management options
Common Skin Conditions
Here are some of the most common skin problems:
- Acne (Acne vulgaris): The most common skin condition, occurring when hair follicles become clogged with oil and dead skin cells. Symptoms include pimples, blackheads, whiteheads, and cysts, often on the face, chest, or back. Hormonal changes during puberty are a primary trigger.
- Eczema (Atopic dermatitis): A chronic condition that causes the skin to be dry, red, inflamed, and intensely itchy. It often appears in childhood and is linked to genetics, allergies, and immune system issues. Triggers can include stress, weather changes, and harsh soaps.
- Psoriasis: An autoimmune disease that speeds up skin cell development, resulting in thick, scaly, and red or silver-colored patches (plaques) on the skin. These patches often form on the elbows, knees, scalp, and lower back and can be itchy or painful.
- Rosacea: A chronic inflammatory condition primarily affecting the face, causing persistent redness, flushing, and sometimes acne-like bumps or visible blood vessels. It is most common in middle-aged adults with fair skin.
- Contact Dermatitis: An inflamed, discolored, and itchy rash caused by an immune reaction to a substance that has touched the skin, such as poison ivy, nickel, or harsh detergents.
- Hives (Urticaria): Raised, red, itchy welts that appear on the skin, often as an allergic reaction to food, medication, or insect stings.
- Fungal Infections (Tinea/Ringworm): Infections like athlete’s foot and jock itch, which thrive in warm, moist areas and cause itchy, red, or scaly patches.
- Warts: Small, rough, raised bumps on the skin caused by the human papillomavirus (HPV).
When to Seek Medical Attention
While many minor skin problems can be managed with over-the-counter treatments and good skincare, you should consult a healthcare provider if you experience:
- A rash that spreads rapidly or does not go away.
- Pain, fever, chills, or shortness of breath accompanying a skin change.
- Open sores, lesions, or blisters that do not heal.
- A change in the size, shape, or color of a mole or new skin growth.
A dermatologist can provide an accurate diagnosis and appropriate treatment plan. More information on specific conditions is available from health resources like the American Academy of Dermatology Association.
Infectious skin diseases For Skin Specialty Course
Infectious skin diseases are caused by various microorganisms, including bacteria, viruses, fungi, and parasites. These conditions can range from mild, easily treatable local infections to severe, potentially life-threatening systemic issues. The infections are often contagious, spreading through direct contact, shared items, or environmental exposure, particularly when the skin’s protective barrier is compromised by a cut or scratch.
Types and Examples of Infectious Skin Diseases
| Type | Examples | Symptoms | Transmission/Cause |
|---|---|---|---|
| Bacterial | Impetigo, Cellulitis, Boils (Furuncles), MRSA | Redness, swelling, pain, pus-filled blisters or sores with honey-colored crusts | Bacteria (commonly Staphylococcus and Streptococcus) enter through breaks in the skin; spread by direct contact or contaminated objects |
| Viral | Warts, Herpes Simplex (cold sores), Shingles, Chickenpox, Hand-Foot-and-Mouth Disease | Bumps, blisters, rashes, itching, tingling, or pain (shingles) | Viruses spread through direct contact with lesions, body fluids (saliva, blister fluid), or the air (chickenpox) |
| Fungal | Ringworm (Athlete’s foot, Jock itch), Yeast Infections (Candidiasis), Nail Fungus | Itching, red or discolored patches (sometimes ring-shaped), scaling, peeling, or brittle nails | Fungi thrive in warm, moist environments; spread through contact with infected people, animals, or contaminated surfaces (e.g., public showers, gym mats) |
| Parasitic | Scabies, Head Lice, Bedbugs | Intense itching (especially at night), rash with small bumps, visible mites or lice/nits (eggs) | Mites or insects burrow into the skin or live in hair; spread through close personal contact, shared bedding, or clothing |
Treatment and Prevention
Treatment depends entirely on the cause of the infection.
- Bacterial infections are typically treated with topical or oral antibiotics.
- Viral infections may use antiviral medications to shorten the duration and severity of symptoms, although some resolve on their own.
- Fungal infections require antifungal creams, powders, or oral medications.
- Parasitic infections are treated with medicated creams or oral medications that kill the mites or lice.
Prevention involves maintaining good personal hygiene (regular handwashing and bathing), keeping wounds clean and covered, avoiding the sharing of personal items (towels, razors, clothing), and avoiding walking barefoot in public damp areas. Vaccinations are also available for some viral infections like chickenpox and shingles
 HRTD Medical Institute
HRTD Medical Institute





