Bronchology
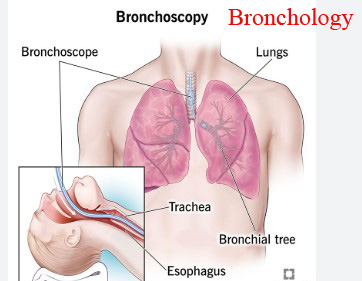
Bronchology. Mobile Phone 01797522136, 01987073965. Bronchology is the branch of medicine focused on the prevention, diagnosis, and treatment of diseases affecting the bronchi, the airways in the lungs. It involves diagnosing and treating conditions like pneumonia, pulmonary fibrosis, and lung cancer, using techniques like bronchoscopy to visualize the airways and take biopsies. Interventional bronchology, a subfield of bronchology, utilizes specialized procedures, including bronchoscopy, to address airway issues, such as stenting and removal of obstructions.
Bronchology is an important subject for PDT Chest Specialty Course, PDT Bronchology Course, PDT Medicine Course, DMDS Course, DMS Course, DMA Course. All these courses are available in HRTD Medical Institute.
Key Aspects of Bronchology
- Diagnosis: Bronchoscopy, which involves inserting a flexible tube with a camera to visualize the airways, is a crucial diagnostic tool.
- Treatment: Interventional bronchology offers various treatments for airway issues, including stenting for narrowing or obstructions, and techniques for managing lung diseases.
- Specialized procedures: Bronchology encompasses a range of procedures, including electromagnetic navigation, robotic bronchoscopy, and endobronchial ultrasound.
- Focus on lung diseases: Bronchology addresses various lung conditions, including pneumonia, pulmonary fibrosis, and allergic reactions.
Diagnosis in Bronchology
In bronchology, diagnosis often involves using bronchoscopy, a procedure where a flexible tube with a camera is inserted into the airways to visualize and sample the lungs. This allows for the identification of abnormal areas, taking tissue biopsies, and evaluating the cause of various lung issues like infections, blockages, and tumors.
Diagnostic Techniques and Their Uses in Bronchology
- Bronchoscopy:
- Visual Inspection: Directly examines the airways for abnormalities like tumors, blockages, or inflammation.
- Biopsy: Tissue samples can be taken from abnormal areas to determine the nature of the lesion (e.g., cancer, infection).
- Bronchoalveolar Lavage (BAL): A sample of fluid is collected from the lungs to identify the cause of infections (e.g., pneumonia, tuberculosis) or other conditions.
- Other Diagnostic Tools:
- Imaging Tests: Chest X-rays and CT scans are used to detect abnormalities that may require further investigation with bronchoscopy.
- Sputum Analysis: Analyzing the mucus produced by the lungs can help diagnose infections.
- Clinical History and Physical Examination: These are crucial in determining the need for and interpretation of bronchoscopy results.
Common Reasons for Bronchoscopy
- Investigating Persistent Symptoms: Cough, hemoptysis (coughing up blood), shortness of breath, or low oxygen levels may necessitate bronchoscopy to determine the underlying cause.
- Following Up on Imaging Abnormalities: If a chest X-ray or CT scan reveals an abnormality, bronchoscopy can be used to further evaluate the area.
- Diagnosing and Treating Airway Blockages:Bronchoscopy can be used to remove foreign bodies or narrowed areas in the airways.
- Assessing and Treating Infections:Bronchoscopy can help diagnose and treat various infections in the lungs, including tuberculosis.
- Evaluating Lung Transplant Rejection:Bronchoscopy can be used to assess for and treat lung rejection after a transplant.
In summary, bronchoscopy is a versatile diagnostic tool that allows for visual examination, tissue sampling, and fluid analysis, making it crucial in the diagnosis and management of a wide range of lung conditions.
Treatment in Bronchology
Bronchology treatment primarily involves bronchoscopy and related interventions to diagnose and treat conditions affecting the airways and lungs, including foreign body removal, airway dilation, tissue biopsy, and tumor ablation. It also includes bronchial toilet, medication like mucolytics and bronchodilators, and in some cases, surgical removal of bronchiectasis.
Bronchoscopy in Bronchology
- Diagnostic: Bronchoscopy allows visualization of the airways, enabling diagnosis of conditions like bronchiectasis, lung cancer, and infections through procedures like bronchoalveolar lavage (BAL) and tissue biopsies.
- Therapeutic: Bronchoscopy can be used to remove foreign objects, clear mucus plugs, dilate narrowed airways, drain abscesses, and even treat certain types of lung cancer.
- Interventional: More advanced techniques like bronchial thermoplasty, stenting, lung volume reduction, and whole lung lavage are performed under bronchoscopic guidance.
Other Bronchology Interventions
- Bronchial Toilet: This involves techniques like coughing up mucus in a specific position to help clear airways.
- Medication: Mucolytics, bronchodilators, and antibiotics are used to manage symptoms and address underlying causes.
- Surgical Removal: In cases where bronchiectasis is severe or refractory to other treatments, surgical removal of the affected lung segments may be an option.
- Electrocautery: This technique uses electricity to treat intraluminal airway lesions.
- Stent Placement: Stents are used to keep airways open, especially in cases of airway stenosis or after tumor removal.
- Laser Therapy: Laser therapy can be used to ablate or debulk endobronchial tumors and control bleeding.
- Brachytherapy: This involves placing a radioactive source directly into the airway to treat localized lung cancer.
- Photodynamic Therapy: This technique uses a light-activated drug to treat endobronchial tumors.
- Whole Lung Lavage: This procedure washes out the lungs with a saline solution to remove accumulated fluid or debris.
Anesthesia for Bronchoscopy
Bronchoscopy can be performed under local anesthesia, moderate sedation, or general anesthesia, depending on the complexity of the procedure and the patient’s needs.
Specialized Procedure in Bronchology
Specialized bronchoscopy procedures extend beyond routine visualization and sampling. These advanced techniques, performed by experienced bronchologists, are used to diagnose and treat a wide range of lung conditions.
Here’s a breakdown of some key specialized bronchoscopy procedures:
1. Endobronchial Ultrasound (EBUS):
- Purpose: EBUS combines bronchoscopy with ultrasound imaging to visualize and biopsy lymph nodes and other structures in the mediastinum (the space between the lungs).
- Application: Used for staging lung cancer, diagnosing mediastinal masses, and obtaining tissue samples for further examination.
2. Navigational Bronchoscopy:
- Purpose: Navigational bronchoscopy uses real-time guidance systems to pinpoint the location of lesions in the lungs, especially those difficult to access with standard bronchoscopy.
- Application: Improves the accuracy of biopsies and allows for more precise targeting of therapeutic interventions.
3. Rigid Bronchoscopy:
- Purpose: Rigid bronchoscopy involves the use of a stiffer, wider scope, allowing for larger-scale procedures and more powerful tools.
- Application: Used for foreign body removal, tumor debulking, stent placement, and other therapeutic procedures in the larger airways.
4. Thermal Techniques (Argon Plasma Coagulation (APC), Electrocautery, Laser, Cryotherapy):
- Purpose:These techniques use heat, cold, or other energy sources to destroy or remove tissues, stop bleeding, or dilate airways.
- Application:Used for airway dilation, tumor destruction, airway bleeding control, and other therapeutic interventions.
5. Endobronchial Brachytherapy:
- Purpose:A radioactive source is placed within the airway to deliver targeted radiation therapy to destroy tumors or prevent recurrence.
- Application:Used for treating airway tumors and can be used in conjunction with other therapies.
6. Airway Stents:
- Purpose: Stents are tubes placed in the airways to keep them open when they are blocked or narrowed by tumors, scar tissue, or other conditions.
- Application: Used to improve breathing in patients with airway obstruction.
7. Bronchial Thermoplasty:
- Purpose: A specialized procedure to reduce smooth muscle tissue in the airways, which can be helpful in some cases of severe asthma.
- Application: Used to manage asthma symptoms and reduce the need for rescue medications.
8. Photodynamic Therapy:
- Purpose: A procedure where a light-sensitive drug is administered, and then activated with a laser, to destroy cancer cells.
- Application: Used to treat certain types of airway tumors.
9. Endoscopic Lung Volume Reduction (ELVR):
- Purpose: A procedure to reduce the size of the lungs, which can be helpful in certain cases of emphysema.
- Application: Used to improve lung function in patients with emphysema.
10. Bronchoalveolar Lavage (BAL):
- Purpose: A procedure to collect fluid from the lungs for analysis, often used to identify infection or other inflammatory conditions.
- Application: Used to diagnose and monitor lung diseases, and can be used in conjunction with bronchoscopy.
These specialized bronchoscopy procedures represent a significant advancement in the diagnosis and treatment of lung diseases, offering more precise and effective approaches to managing complex conditions.
Common Lung Diseases
The most common and well-known lung diseases include asthma, COPD, pneumonia, lung cancer, pulmonary fibrosis, etc.
- Asthma: A chronic inflammatory disorder of the airways, causing difficulty breathing.
- COPD (Chronic Obstructive Pulmonary Disease): A group of lung diseases that block airflow and make it difficult to breathe.
- Pneumonia: An infection of the lungs, often caused by bacteria or viruses.
- Lung Cancer: The uncontrolled growth of abnormal cells in the lungs.
- Pulmonary Fibrosis: Scarring and thickening of the lung tissue.
- Bronchitis: Inflammation of the bronchial tubes.
- Emphysema: A type of COPD where the air sacs in the lungs are damaged.
- Mesothelioma: A cancer caused by asbestos exposure, primarily affecting the lining of the lungs.
- Pulmonary Edema: Fluid buildup in the lungs.
- Pulmonary Hypertension: High blood pressure in the arteries of the lungs.
Other Lung Diseases:
- Pulmonary Embolism: A blood clot that travels to the lungs and blocks an artery.
- Sarcoidosis: A condition where abnormal collections of inflammatory cells (granulomas) form in various organs, including the lungs.
- Tuberculosis (TB): A contagious bacterial infection that primarily affects the lungs.
- Bronchiectasis: A condition where the airways of the lungs become widened and damaged.
- Cystic Fibrosis: A genetic disorder that affects the lungs and other organs.
Asthma
Asthma is a chronic respiratory condition characterized by airway inflammation and narrowing, leading to symptoms like coughing, wheezing, and shortness of breath. It’s triggered by various factors and can range from mild to severe. Diagnosis involves a combination of medical history, physical exam, and lung function tests. Treatment focuses on controlling symptoms and preventing exacerbations using medications and lifestyle modifications.
Causes:
Asthma is a complex condition with both genetic and environmental factors playing a role. Common triggers include:
- Allergens: Pollen, dust mites, pet dander, and mold.
- Irritants: Smoke, pollutants, and strong chemicals.
- Exercise: Can trigger asthma symptoms in some individuals.
- Infections: Viral respiratory infections can worsen asthma.
- Other Factors: Cold air, certain medications, and strong emotions can also trigger symptoms.
Clinical Features:
The main symptoms of asthma include:
- Coughing: Especially at night or after exercise.
- Wheezing: A whistling sound when breathing out.
- Shortness of breath: Difficulty breathing, even at rest.
- Chest tightness or pain: Feeling of pressure or discomfort in the chest.
Diagnosis:
A diagnosis of asthma is typically made based on:
- Medical history: Including family history of asthma and allergies.
- Physical examination: Assessing symptoms and lung sounds.
- Lung function tests: Such as spirometry (measuring how much air you can breathe out) and FeNO test (measuring nitric oxide in your breath, which indicates inflammation).
Investigation:
- Spirometry: Measures lung capacity and airflow.
- FeNO test: Measures the amount of nitric oxide in exhaled breath, which can indicate inflammation in the airways.
- Other tests: May include allergy testing, chest X-rays, and blood tests to rule out other conditions.
Treatment:
Treatment aims to control symptoms and prevent asthma attacks:
- Medications:
- Quick-relief medications: Bronchodilators (like albuterol) that open the airways.
- Long-term control medications: Inhaled corticosteroids (like fluticasone) that reduce inflammation.
- Other medications: Leukotriene modifiers and biologics may be used in certain cases.
- Asthma action plan: A personalized plan that outlines when and how to use medications and when to seek medical attention.
- Lifestyle modifications: Avoiding triggers, staying active, and maintaining a healthy weight.
Complications:
- Asthma attacks: Severe episodes of shortness of breath and wheezing that can require hospitalization.
- Respiratory failure: Severe cases can lead to respiratory failure, where the lungs cannot provide enough oxygen to the blood.
- Lung damage: Chronic inflammation can damage the lungs over time.
Prevention:
- Avoid triggers: Identify and avoid allergens, irritants, and other triggers.
- Follow asthma action plan: Use medications as prescribed and seek medical attention when needed.
- Manage underlying conditions: Control allergies, eczema, and other conditions that can worsen asthma.
- Stay active: Regular exercise can improve lung function and reduce asthma symptoms.
- Stay healthy: Maintain a healthy weight, control heartburn, and avoid smoking.
COPD
COPD is a chronic, progressive lung disease characterized by airflow obstruction and lung damage, most often caused by smoking. Symptoms include shortness of breath, cough, and wheezing, and diagnosis is confirmed by spirometry. Treatment focuses on symptom management, preventing exacerbations, and slowing disease progression through medication, pulmonary rehabilitation, and potentially surgery.
Causes of COPD:
- Smoking: The most significant risk factor, according to the NHS.
- Alpha-1 antitrypsin deficiency: A rare genetic condition that predisposes individuals to lung damage.
- Occupational exposures: Exposure to certain dusts, fumes, or chemicals can increase COPD risk.
- Air pollution: Long-term exposure to air pollution can contribute to COPD development.
- Secondhand smoke: Exposure to secondhand smoke can also increase the risk of COPD.
- Family history: A family history of COPD can increase an individual’s risk.
Clinical Features of COPD:
- Shortness of breath: Difficulty breathing, especially during physical activity.
- Chronic cough: A persistent cough, often producing mucus.
- Wheezing: A whistling sound when breathing.
- Chest tightness: A sensation of tightness or pressure in the chest.
- Fatigue: Feeling tired or lacking energy.
- Progressive shortness of breath: Breathing difficulties worsen over time.
Diagnosis of COPD:
- Spirometry: A lung function test that measures how much air you can breathe in and out and how fast you can blow it out, confirming the diagnosis of COPD.
- Chest X-ray: Can rule out other lung conditions.
- Medical history and physical examination: A doctor will assess symptoms, medical history, and perform a physical exam.
Investigations for COPD:
- Pulse oximetry: Measures oxygen levels in the blood.
- Arterial blood gas test: Measures oxygen and carbon dioxide levels in the blood.
- Electrocardiogram (ECG): Checks for heart-related problems, which can be common in COPD.
- Exercise testing: Evaluates lung function during exercise.
- Blood tests: Can help identify other underlying conditions.
Treatment of COPD:
- Smoking cessation: The most important step in managing COPD is to quit smoking.
- Medications:
- Bronchodilators: Help relax airway muscles, making breathing easier.
- Inhaled corticosteroids: Reduce inflammation in the airways.
- Antibiotics: Used to treat respiratory infections.
- Pulmonary rehabilitation: A program of exercise and education to improve lung function and manage COPD symptoms.
- Supplemental oxygen: Used when oxygen levels in the blood are low.
- Non-invasive ventilation (NIV): Provides breathing assistance through a mask or other device.
- Surgery: Lung volume reduction surgery or lung transplantation may be considered in severe cases.
Complications of COPD:
- Respiratory infections: COPD increases the risk of developing respiratory infections like pneumonia.
- Heart problems: COPD can cause heart failure or high blood pressure in the lung arteries.
- Lung cancer: Smokers with COPD have a higher risk of lung cancer.
- Mental health problems: COPD can lead to depression and anxiety.
Prevention of COPD:
- Do not smoke: Avoid smoking or quitting if you smoke.
- Avoid exposure to irritants: Minimize exposure to air pollution, dust, fumes, and secondhand smoke.
- Stay up-to-date on vaccines: Get vaccinated against the flu and pneumonia.
Pneumonia
Pneumonia, a lung infection, is caused by bacteria, viruses, or fungi, leading to inflammation and fluid buildup in the lungs. Symptoms can range from mild to severe, including cough, fever, difficulty breathing, and chest pain. Diagnosis typically involves a physical exam and chest X-ray. Treatment focuses on addressing the cause, with antibiotics for bacterial pneumonia, and antiviral or antifungal medications for viral or fungal cases. Complications can be serious, and prevention includes vaccination and healthy habits.
Causes:
- Bacteria:Common causes include Streptococcus pneumoniae and Haemophilus influenzae.
- Viruses:Respiratory viruses like influenza and the coronavirus SARS-CoV-2 can cause pneumonia.
- Fungi:Less common, but fungi can also be a cause, particularly in individuals with weakened immune systems.
- Other:Pneumonia can also develop after aspiration (inhaling foreign material) or due to underlying health conditions.
Clinical Features (Symptoms):
- General:Fever, chills, sweating, fatigue, loss of appetite, and muscle aches.
- Respiratory:Cough (may produce mucus), shortness of breath, rapid breathing, and chest pain when breathing or coughing.
- Other:Nausea, vomiting, confusion (especially in older adults), and bluish discoloration of lips or fingernails.
- Severity:Symptoms can vary, with some cases being mild and others progressing to severe, life-threatening pneumonia.
Diagnosis:
- Physical exam:Doctors assess symptoms, medical history, and may listen to the chest with a stethoscope.
- Chest X-ray:This imaging test can confirm pneumonia and show the extent of the infection.
- Blood tests:A complete blood count (CBC) can help determine the presence of infection, and a pulse oximetry can measure blood oxygen levels.
- Other tests:In some cases, a chest CT scan or sputum culture may be ordered.
Treatment:
- Antibiotics: Used for bacterial pneumonia, usually prescribed for 5-7 days.
- Antiviral medications: Used for viral pneumonia, like influenza or COVID-19.
- Antifungal medications: Used for fungal pneumonia.
- Supportive care: Includes oxygen therapy, fluids, and pain relief medications.
- Hospitalization: May be necessary for severe cases requiring intravenous antibiotics and other advanced treatments.
Complications:
- Severe illness: Pneumonia can lead to breathing difficulties, sepsis (a life-threatening infection), and other serious complications.
- Lung damage: In some cases, pneumonia can cause permanent lung damage.
- Mortality: Pneumonia can be fatal, especially in vulnerable populations like infants, the elderly, and individuals with weakened immune systems.
Prevention:
- Vaccinations: The pneumococcal and influenza vaccines help protect against pneumonia.
- Healthy habits: Maintaining good hygiene (hand washing), quitting smoking, and staying active help strengthen the immune system.
- Avoid exposure: Avoiding contact with individuals who have respiratory infections and practicing respiratory etiquette (covering coughs and sneezes) can help reduce the spread of pneumonia.
- Get vaccinated: The CDC recommends getting vaccinated against pneumococcal and influenza viruses.
- Practice good hygiene: Washing hands frequently, especially after coughing or sneezing, can help prevent the spread of germs that cause pneumonia.
- Stay away from people who are sick: If you are ill, stay home to avoid infecting others.
- Eat a healthy diet: Maintaining a balanced diet can help support your immune system.
- Exercise regularly: Regular physical activity can help strengthen your immune system and reduce your risk of pneumonia.
- Don’t smoke: Smoking damages your lungs and makes you more susceptible to pneumonia.
Bronchitis
Bronchitis, a condition causing airway inflammation, can be acute (short-term) or chronic (long-term). It’s typically characterized by a cough that may bring up mucus, and can be caused by infections or irritants. Diagnosis relies on medical history, physical exam, and possibly tests like X-rays. Treatment focuses on managing symptoms, which may include rest, hydration, and in some cases, medications like bronchodilators or steroids. Complications can include pneumonia, and prevention involves avoiding smoking and irritants, along with vaccinations against pneumonia and the flu.
Causes:
- Infections: Bronchitis can be caused by viral or bacterial infections.
- Irritants: Exposure to irritants like smoke, chemicals, or pollutants can trigger bronchitis.
- Smoking: Smoking is a major risk factor for both acute and chronic bronchitis.
Clinical Features (Symptoms):
- Cough: A persistent cough that can produce mucus.
- Wheezing: A whistling sound when breathing.
- Shortness of breath: Difficulty breathing.
- Chest discomfort: Pain or tightness in the chest.
- Other symptoms: Runny or blocked nose, headache, fever, and aches and pains may also be present.
Diagnosis:
- Medical history and physical exam: A doctor will ask about symptoms and listen to your lungs.
- Chest X-ray: This can help rule out pneumonia or other conditions.
- Blood tests: May be used to assess for infections or other underlying conditions.
Treatment:
- Rest: Getting enough rest is important to allow the body to heal.
- Hydration: Drinking plenty of fluids helps thin mucus.
- Medications:
- Bronchodilators: Help open up the airways.
- Steroids: Reduce inflammation.
- Antibiotics: May be prescribed if a bacterial infection is suspected.
- Other measures: Using a humidifier, avoiding irritants, and potentially wearing a mask.
Complications:
- Pneumonia: If the infection spreads to the lungs.
- Worsening of other conditions: Bronchitis can worsen asthma or other respiratory conditions.
Prevention:
- Avoid smoking: Quitting smoking is essential.
- Avoid irritants: Minimize exposure to smoke, dust, fumes, and air pollution.
- Vaccinations: Get vaccinated against pneumonia and the flu.
- Wash your hands: Frequently wash your hands to reduce the spread of germs.
- Manage other conditions: If you have asthma or other conditions, manage them effectively.
Pulmonary Fibrosis
Pulmonary fibrosis is a chronic, progressive disease characterized by scarring and thickening of the lung tissue. This scarring hinders the lungs’ ability to exchange oxygen, leading to shortness of breath, a dry cough, and other symptoms. Diagnosis involves a combination of medical history, imaging (CT scan), lung function tests, and potentially a lung biopsy. Treatment focuses on symptom management and slowing disease progression, with medications like nintedanib and pirfenidone, oxygen therapy, pulmonary rehabilitation, and lung transplant options.
Causes and Risk Factors:
- Idiopathic Pulmonary Fibrosis (IPF): In many cases, the cause is unknown.
- Environmental Factors: Exposure to certain substances like asbestos, silica, or dust can trigger lung damage.
- Medications: Some medications can cause lung scarring as a side effect.
- Radiation Therapy: Radiation treatments for chest conditions can also damage lung tissue.
- Underlying Conditions: Certain autoimmune diseases, inflammatory conditions, and infections can contribute to pulmonary fibrosis.
- Family History: A family history of pulmonary fibrosis can increase risk.
Clinical Features:
- Shortness of Breath: Gradual worsening breathlessness, especially with exertion.
- Dry Cough: A persistent, nonproductive cough.
- Fatigue and Weight Loss: General tiredness and unintentional weight loss are common.
- Clubbing of Fingers/Toes: Enlarged finger and toe tips due to lack of oxygen.
- Joint and Muscle Pain: Arthralgia and myalgia may be present.
Diagnosis and Investigation:
- Medical History and Examination: Detailed assessment of symptoms, exposure history, and family history.
- Chest X-ray and CT Scan: Imaging to identify lung scarring and patterns of damage.
- Lung Function Tests (Pulmonary Function Tests): Evaluate lung capacity and gas exchange, often showing a restrictive pattern.
- Lung Biopsy: In some cases, a lung biopsy may be needed to confirm the diagnosis and rule out other conditions.
- Blood Tests: Assess for underlying systemic diseases or inflammation.
Treatment and Management:
- Medications:
- Antifibrotic Drugs: Nintedanib and pirfenidone can help slow down the progression of scarring.
- Oxygen Therapy: Supplemental oxygen may be needed to address shortness of breath and maintain oxygen levels.
- Pulmonary Rehabilitation:Exercises and techniques to improve lung function, exercise tolerance, and quality of life.
- Lung Transplant:In severe cases, lung transplant may be an option.
- Supportive Care:Addressing symptoms, managing complications, and improving quality of life.
Complications:
- Pulmonary Hypertension: High blood pressure in the pulmonary arteries.
- Respiratory Failure: Inability of the lungs to adequately exchange oxygen and carbon dioxide.
- Pneumothorax: Collapse of the lung.
- Lung Cancer: Increased risk of lung cancer.
Prevention and Lifestyle Modifications:
- Avoid Lung Irritants: Reduce exposure to dust, chemicals, and secondhand smoke.
- Smoking Cessation: Quitting smoking is crucial.
- Vaccinations: Stay up-to-date on vaccines, including influenza and pneumonia vaccines.
- Healthy Lifestyle: Maintain a healthy weight, eat a balanced diet, and engage in regular exercise.
Lung Cancer
Lung cancer, a leading cause of cancer-related deaths, is primarily caused by smoking. Clinical features include persistent cough, shortness of breath, and chest pain. Diagnosis involves chest X-rays, CT scans, and biopsies. Treatment options include surgery, chemotherapy, and radiation therapy. Complications can include fluid buildup in the chest and spread to other body parts. Prevention focuses on quitting smoking and avoiding exposure to carcinogens.
1. Causes:
- Smoking: Cigarette smoking is the primary cause of lung cancer, responsible for about 85% of cases.
- Exposure to Carcinogens: Radon, asbestos, and other occupational chemicals also increase the risk.
- Other Factors: Family history, certain lung diseases, and radiation therapy can also contribute to lung cancer risk.
2. Clinical Features (Symptoms):
- Persistent Cough: A cough that doesn’t go away or gets worse.
- Shortness of Breath: Difficulty breathing or a feeling of being winded.
- Chest Pain: Pain in the chest that may worsen with breathing or coughing.
- Other Symptoms: Coughing up blood, hoarseness, fatigue, weight loss, and loss of appetite.
3. Diagnosis:
- Imaging: Chest X-rays and CT scans are used to detect tumors and assess their size and location.
- Biopsy: A sample of lung tissue is taken for examination under a microscope to confirm the presence of cancer cells.
- Other Tests: Bronchoscopy, sputum cytology, and lung function tests may also be used.
4. Investigations:
- Imaging Studies:CT scans and PET scans can help determine the extent of the cancer and whether it has spread to other parts of the body.
- Biopsy:Different types of biopsies, including needle biopsies and bronchoscopy, are used to obtain tissue samples for analysis.
- Blood Tests:Blood tests can help assess overall health and rule out other possible causes of symptoms.
5. Treatment:
- Surgery: If the cancer is localized, surgery can remove the tumor.
- Chemotherapy: Drugs are used to kill cancer cells throughout the body.
- Radiation Therapy: High-energy rays are used to kill cancer cells and shrink tumors.
- Targeted Therapy: Drugs that target specific proteins or genes involved in cancer growth are used.
- Immunotherapy: Drugs that boost the body’s immune system to fight cancer cells are used.
6. Complications:
- Fluid in the Chest: Lung cancer can cause fluid to accumulate in the chest cavity, leading to shortness of breath.
- Spread of Cancer: Lung cancer can spread to other parts of the body, including the brain, liver, and bones.
- Infections: Lung cancer can increase the risk of infections, especially pneumonia.
- Blood Clots: Lung cancer can increase the risk of blood clots in the legs or lungs.
7. Prevention:
- Quit Smoking: The most effective way to prevent lung cancer is to quit smoking or never start.
- Avoid Secondhand Smoke: Exposure to secondhand smoke also increases the risk of lung cancer.
- Reduce Exposure to Carcinogens: Avoid or minimize exposure to asbestos, radon, and other chemicals.
- Regular Checkups: High-risk individuals should undergo regular screenings for lung cancer.
- Healthy Lifestyle: Maintaining a healthy diet, exercising regularly, and managing stress can also help reduce the risk of lung cancer.
Emphysema
Emphysema, a form of chronic obstructive pulmonary disease (COPD), is characterized by damage to the air sacs (alveoli) in the lungs, leading to shortness of breath and difficulty breathing. Smoking is the most common cause, but other factors like air pollution and genetic predisposition can also contribute. Diagnosis involves medical history, physical examination, lung function tests, and imaging. Treatment focuses on managing symptoms, preventing complications, and slowing disease progression through medications, smoking cessation, and pulmonary rehabilitation.
Causes:
- Smoking: The primary cause, leading to alveolar damage and inflammation.
- Air pollution: Exposure to pollutants can damage the lungs and contribute to emphysema.
- Chemical fumes: Prolonged exposure to certain chemicals can also damage lung tissue.
- Genetic factors: Alpha-1 antitrypsin deficiency can increase the risk of developing early-onset emphysema.
- Other factors: Age, gender, and previous lung diseases can also play a role.
Clinical Features (Symptoms):
- Shortness of breath: Difficulty breathing, especially with exertion, which may progress to shortness of breath even at rest.
- Chronic cough: Persistent cough, often producing mucus.
- Wheezing: A whistling sound during exhalation.
- Chest tightness: Feeling of pressure or constriction in the chest.
- Fatigue: Increased tiredness due to the effort of breathing.
- Other: Weight loss, ankle swelling, and frequent respiratory infections.
Diagnosis:
- Medical history: Includes a detailed account of symptoms, smoking history, and family history.
- Physical examination: Assessing lung sounds, breathing patterns, and overall health.
- Lung function tests: Spirometry and other tests to measure lung capacity and airflow.
- Imaging tests: Chest X-rays or CT scans to visualize the lungs and identify damage.
- Blood tests: To evaluate oxygen levels and identify other health issues.
Investigations:
- Spirometry: Measures the amount and speed of air expelled from the lungs.
- Chest X-ray or CT scan: Visualizes lung structure and can identify emphysema-related changes.
- Arterial blood gas test: Measures oxygen and carbon dioxide levels in the blood.
- Pulse oximetry: Measures oxygen saturation in the blood.
- Electrocardiogram (ECG): Evaluates heart function.
Treatment:
- Smoking cessation: The most important step in slowing disease progression.
- Medications: Bronchodilators, corticosteroids, and other drugs to help with breathing and inflammation.
- Pulmonary rehabilitation: A program that combines exercise, education, and counseling to improve breathing and quality of life.
- Oxygen therapy: May be needed in advanced stages of the disease.
- Surgery: Lung volume reduction surgery or lung transplantation may be considered in severe cases.
Complications:
- Frequent respiratory infections: Colds and pneumonia can be more common in people with emphysema.
- Heart problems: Emphysema can put a strain on the heart and lead to heart failure.
- Hypoxemia: Low blood oxygen levels.
- Hypercapnia: High carbon dioxide levels in the blood.
- Lung collapse (pneumothorax): Emphysema can weaken the lung tissue, making it more prone to collapse.
Prevention:
- Avoid smoking: Quitting smoking is the most effective way to prevent emphysema.
- Minimize exposure to pollutants: Avoid areas with high levels of air pollution and chemical fumes.
- Early detection and management: Regular check-ups and prompt treatment of respiratory infections can help slow the progression of emphysema.
- Healthy lifestyle: Maintaining a healthy weight, eating a nutritious diet, and engaging in regular exercise can improve overall lung health.
Mesothelioma
Mesothelioma, a rare cancer, develops in the lining of the lungs, abdomen, heart, or testicles, primarily due to asbestos exposure. Symptoms include shortness of breath, chest pain, abdominal swelling, and weight loss. Diagnosis involves imaging tests, blood tests, and biopsies, while treatment options include surgery, chemotherapy, radiation, and immunotherapy. Prevention focuses on avoiding asbestos exposure.
Causes:
- Mesothelioma is almost always caused by exposure to asbestos, a group of naturally occurring minerals with microscopic fibers.
- Asbestos was widely used in construction and manufacturing before its hazards were recognized.
- Exposure can occur through inhalation or swallowing asbestos fibers, which can be released when working with asbestos-containing materials.
- Exposure can lead to mesothelioma development between 20 and 60 years after exposure.
- People at higher risk include builders, plumbers, electricians, welders, asbestos miners, and those working in the automotive and textile industries.
Clinical Features (Symptoms):
- Pleural Mesothelioma: Chest pain, shortness of breath, cough (often dry), and difficulty breathing.
- Peritoneal Mesothelioma: Abdominal pain, swelling, fluid buildup, loss of appetite, nausea, and vomiting.
- Other Mesothelioma: Fatigue, weight loss, fever, and night sweats.
- Pericardial Mesothelioma: Chest pain, shortness of breath, and potential heart rhythm abnormalities.
Diagnosis:
- Imaging tests: X-rays, CT scans, MRI, and PET scans are used to detect fluid accumulation and tumor location.
- Blood tests: Look for biomarkers (e.g., SMRP, MPF, CA125, Fibulin-3) that may be elevated in mesothelioma.
- Biopsies: Tissue samples are taken to confirm the diagnosis and determine the cell type of mesothelioma.
Investigations:
- Imaging Tests:X-rays, CT scans, MRI, and PET scans are used to visualize the tumor and assess its extent.
- Blood Tests:These tests help assess overall health, organ function, and look for cancer-related biomarkers.
- Biopsies:A tissue sample is taken and examined under a microscope to confirm the diagnosis and determine the type of mesothelioma.
Treatment:
- Surgery: May be an option for some patients with localized disease.
- Chemotherapy: Involves using drugs to kill cancer cells.
- Radiation Therapy: Uses radiation to target and destroy cancer cells.
- Immunotherapy: Uses the body’s immune system to fight cancer.
- Targeted Therapies: Target specific molecules in cancer cells.
- Clinical Trials: Offer opportunities for patients to participate in research studies on new treatments.
Complications:
- Fluid Buildup:Can cause breathing difficulties (pleural effusion) or abdominal discomfort (ascites).
- Spread of Cancer:Mesothelioma can spread to other parts of the body, leading to further complications.
- Treatment Side Effects:Chemotherapy and radiation can cause side effects such as fatigue, nausea, and hair loss.
- Other Complications:Depending on the site of the mesothelioma, complications can include bowel obstruction, pneumonia, and blood clots.
Prevention:
- Avoid Asbestos: The primary way to prevent mesothelioma is to avoid exposure to asbestos.
- Protect Yourself: Wear protective gear and follow safety precautions when working with asbestos.
- Be Aware: If you suspect you have asbestos in your home, consult a professional for assessment and mitigation.
Pulmonary Edema
Pulmonary edema, an abnormal buildup of fluid in the lungs, can be caused by heart problems or other medical conditions. Symptoms include difficulty breathing, coughing up blood or frothy mucus, and wheezing. Diagnosis involves assessing symptoms, conducting chest X-rays, blood tests, and potentially ECGs or echocardiograms. Treatment focuses on managing the underlying cause, providing oxygen support, and potentially using medications to reduce fluid or improve breathing.
Causes:
- Cardiogenic pulmonary edema:This type is most commonly caused by heart failure, where the heart is unable to pump blood efficiently, leading to fluid buildup in the lungs.
- Non-cardiogenic pulmonary edema:This type can result from various conditions, including pneumonia, trauma, exposure to certain toxins, or high-altitude exposure.
Clinical Features:
- Shortness of breath: This is a hallmark symptom, often worsening when lying down (orthopnea).
- Coughing up blood or frothy mucus: This can be a sign of fluid buildup in the lungs.
- Wheezing: A high-pitched whistling sound during breathing.
- Chest tightness or pain: Can accompany the shortness of breath.
- Feeling of suffocation: A sense of being unable to breathe adequately.
- Swelling in the legs: Fluid buildup can also affect other parts of the body.
- Anxiety or restlessness: Can occur due to shortness of breath.
- Excessive sweating: A symptom of the body struggling to maintain balance.
- Blueish tinge of lips or fingers: This indicates low oxygen levels.
Diagnosis:
- Patient history and physical examination: A detailed assessment of the patient’s symptoms and medical history.
- Chest X-ray: Can reveal the presence of fluid in the lungs.
- Blood tests: To assess oxygen and carbon dioxide levels, as well as other indicators of lung function.
- Electrocardiogram (ECG): To evaluate heart function and identify any abnormalities.
- Echocardiogram: Can provide a more detailed view of heart structure and function.
Investigation:
- Pulmonary Function Tests (PFTs): To assess lung capacity and airflow.
- Arterial Blood Gas (ABG) analysis: To determine blood oxygen and carbon dioxide levels.
- Sputum analysis: To identify any infection causing the edema.
Treatment:
- Supplemental oxygen: To help the body receive more oxygen.
- Medications:
- Diuretics: To help the body eliminate excess fluid.
- Vasodilators: To relax blood vessels and reduce pressure in the heart.
- Inotropes: To help the heart pump more effectively.
- Other medications: To address underlying conditions such as heart failure, high blood pressure, or infections.
- Mechanical ventilation: May be necessary in severe cases to support breathing.
- Monitoring and supportive care: To ensure the patient’s well-being and manage any complications.
Complications:
- Acute respiratory distress syndrome (ARDS): A serious lung injury that can result from prolonged edema.
- Organ failure: Prolonged oxygen deprivation can lead to dysfunction in multiple organ systems.
- Death: In severe cases, pulmonary edema can be fatal without prompt treatment.
Prevention:
- Manage underlying conditions: Such as heart failure, hypertension, and respiratory infections.
- Lifestyle modifications: Including a heart-healthy diet, regular exercise, and avoiding smoking.
- Take medications as directed: If you have a heart condition.
- Get routine vaccinations: To prevent infections.
- See your healthcare provider regularly: For checkups and to address any concerns.
Pulmonary Hypertension
Pulmonary hypertension (PH) is a serious condition characterized by high blood pressure in the pulmonary arteries, leading to shortness of breath, fatigue, and potentially heart failure. Causes range from genetic factors and heart or lung diseases to other conditions and even certain drugs. Diagnosis involves a combination of physical exams, echocardiograms, and potentially right heart catheterization. Treatment focuses on managing symptoms and underlying causes, including medications, oxygen therapy, and in some cases, surgery. Complications include heart failure and death. Prevention strategies include managing underlying conditions, avoiding high-risk drugs, and early detection.
Causes:
- Unknown (Idiopathic): The cause is not known.
- Genetic: Inherited from family members.
- Heart Disease: Conditions like left-sided heart failure can cause PH.
- Lung Disease: Conditions like COPD, interstitial lung disease, or sleep apnea can contribute.
- Other Conditions: Liver disease, sickle cell disease, blood clots in the lungs, and connective tissue disorders can also be factors.
- Medications and Drugs: Some medications, including those used for diet, and illicit drugs can increase the risk.
Clinical Features:
- Shortness of breath: Especially with exertion.
- Fatigue: Feeling tired and weak.
- Dizziness and fainting: Due to reduced blood flow to the brain.
- Chest pain: Can be a symptom of increased pressure in the pulmonary arteries.
- Swelling: In the legs, ankles, and feet due to fluid buildup.
- Right-sided heart failure symptoms: As the condition progresses, right-sided heart failure can develop.
Diagnosis:
- Physical Exam: Doctors will assess symptoms and listen to the heart and lungs.
- Echocardiogram: An ultrasound of the heart to visualize blood flow and assess heart function.
- Blood Tests: Can help identify underlying conditions and complications.
- Chest X-ray: Provides a picture of the lungs and heart.
- Right Heart Catheterization: A procedure to measure the pressure in the pulmonary arteries, often used for definitive diagnosis.
Investigations:
- Echocardiogram: Provides an image of the heart and estimates pressure in the pulmonary arteries.
- Right Heart Catheterization: Measures blood pressure in the pulmonary arteries.
- Blood Tests: Help identify underlying conditions and complications.
- Electrocardiogram (ECG): Records the electrical activity of the heart.
- Chest X-ray: Visualizes the lungs and heart.
- Pulmonary Function Tests: Assess lung function.
Treatment:
- Medications:
- Anticoagulants: Help prevent blood clots.
- Diuretics: Help remove excess fluid.
- Vasodilators: Help widen blood vessels.
- Specific Medications: For pulmonary arterial hypertension (PAH).
- Oxygen Therapy: Provides supplemental oxygen to improve blood oxygen levels.
- Surgery: In some cases, surgery may be needed.
- Managing Underlying Conditions: Addressing the underlying cause of PH.
Complications:
- Right-sided heart failure: Can develop due to the heart working harder.
- Heart failure: Can lead to a weakened heart.
- Death: In severe cases, PH can be life-threatening.
- Reduced Quality of Life: Symptoms can significantly impact daily activities.
Prevention:
- Manage Underlying Conditions: Treat heart and lung diseases, as well as other conditions that can lead to PH.
- Avoid High-Risk Drugs: Avoid substances that can damage pulmonary arteries.
- Early Detection and Treatment: Early diagnosis and treatment can improve outcomes.
 HRTD Medical Institute
HRTD Medical Institute




