General Pathology Details
General Pathology. Mobile Phone Number 01797522136, 01987073965. General Pathology is a branch of pathology that discusses the known clinical abnormalities of disease.
General Pathology includes atrophy, hypertrophy, metaplasia, gangrene, etc. General Pathology is important for understanding the causes and procedures of disease. General Pathology is a common subject in Medical Science. There are many courses at HRTD Medical Institute where General Pathology is Mandatory for study. These courses are Paramedical, DMA, DMS, DMDS, Diploma in Pathology, Diploma in Dental, Diploma in Nursing, Diploma in Physiotherapy, etc.
Definition of Pathology
The word pathology comes from two Greek words,
Pathos-suffering,
Logos- knowledge.
So literally pathology means the study of suffering.
It is the branch of medical science that deals with the study of structural and functional changes in cells, tissues, and organs in diseases.
Definition of General Pathology
General Pathology is a branch of pathology that discusses the known clinical abnormalities of disease. General Pathology includes atrophy, hypertrophy, metaplasia, gangrene, etc.
Area of study of pathology
Basically, pathology discusses four aspects of a disease
✓ The cause (etiology)
✓ The mechanisms of its development (pathogenesis)
✓ The structural alterations induced in the cells, tissues, and organs (morphologic changes)
✓ The functional consequences of the morphologic changes, (clinical significance)
Branches of pathology
The branches of pathology can be summarized as –

- General pathology: Concern with the basic reaction of cells and tissues to abnormal stimuli that underlie all diseases. It includes discussions about inflammation, cell injury, neoplasm, etc.
- Systemic or special pathology: Concern with the specific response of specialized organs and tissues to or less well-defined stimuli. It includes discussion about systemic diseases such as dermatitis, appendicitis, aplastic anemia, etc.
- Clinical pathology: Concern with biochemical and microbiological procedures performed on collected tissues or other substances to determine the changes in relation to disease. e.g. examination of blood, urine, etc.
GENERAL ASPECTS OF DISEASE
The word disease comes from two words Dis- no, Ease- comfort. So the term “Disease” literally means “without Ease” (uneasiness or, uncomfort).
The disease can be defined as a condition of the body of some part or organ of the body in which the functions are disturbed or deranged.
Causes of disease
The causes of disease can be summarized as
- Hereditary or Genetic cause; (e.g. in psoriasis.)
- Congenital cause; (e.g in ophthalmia neonatorum. )
- Biological cause e.g. bacteria, virus, protozoa, fungus etc.
- Physical cause e.g. Trauma, heat, cold, foreign body.
- Chemical agents; e.g. toxic substances.
- Nutritional imbalances; e.g. iron deficiency, iodine deficiency, protein deficiency, vitamin deficiency, etc.
- Immunological; e.g. hypersensitivity reaction, allergic reaction etc. (e.g. in Bronchial asthma, )
- Metabolic cause: (e.g. in uremia, diabetes mellitus.)
- Psychogenic cause; (e.g. in peptic ulcer)
- iatrogenic cause; (e.g. in anaphylaxis due to antibiotic injection.)
- Idiopathic cause; (e.g. Crohn’s disease, ulcerative
- colitis)
Classification of disease
The disease can be classified in many ways. E.g.
- Based on site: e.g. disease of the respiratory system, cardiovascular disease, disease of blood, etc.
- Based on pathology: e.g. inflammatory disease, degenerative disease, neoplastic disease, etc.
- Based on the cause: e.g. bacterial disease, viral disease, etc.
- Based on communicability: e.g. communicable disease, noncommunicable disease etc.
- Based on duration; it can be
- Acute: short duration. Occurs suddenly and changes are rapid. A few hours to a few days. E.g. influenza.
- Chronic: long duration. Changes take place slowly. e.g. tuberculosis.
- Acute: on chronic: these are chronic but sometimes acute exacerbation takes place. e.g. chronic hepatitis B makes changes in the liver slowly but occasionally makes rapid changes nad manifested by clinical signs and symptoms.
Expression of disease
Expression of disease can be in three ways-
- By sign: these expressions can be felt by physician or attendance, e.g., fever, cough etc. A single sign can be expression of many pathological state. Such as- fever can be sign of respiratory, urinary, nervous system etc disorders.
- Symptoms such manifestation only felt by patient himself. e.g. pain. A single symptom also can be expression of many pathological state. Such as abdominal pain can be symptom of digestive, urinary, reproductive system etc. disorder.
- Internal changes: in some cases it can be felt from outside of body. But in most cases these cannot be identified by patient or physician; e.g. kidney damage. These changes can be identified only by pathological investigations. Some pathological changes indicate a specific disease and some changes may indicate various non specific disorders.
Generally sign and symptom makes clinical feature of disease.
When clinical feature appears than pathological investigation is done to confirm the disease.
CELL & ITS STRUCTURE
The cell is the structural and functional unit of a living being.
The human body is built up of various types of cells. Generally, the size of the cells varies from 5-50 nanometers (but maybe larger). A recent research article found that the total number of cells (of a 30-year-old and 70 kg body weight & body 1.85 m²) is about 3.72 X 10¹3.
All the body functions are performed and maintained by different types of cells. The abnormal function of cells leads to a pathological state.
Composition of cell
Average composition of human cells –
| Percent of Mass | |
| Water | 65 |
| Other Inorganic | 1.5 |
| Protein | 20 |
| Lipids | 12 |
| RNA | 1.0 |
| DNA | 0.1 |
| Other Organics | 0.4 |
Figure: Structures of Human cell
Components of cell
- Cell membrane
- Protoplasm
- Nucleus
- Cytoplasm
- Organelles
- Membranous: e.g. Mitochondria, Endoplasmic reticulum, Golgi complex, Lysosomes, Peroxisomes
- Nonmembranous: e.g. Ribosome, Centrosome, Microfilament, Microtubules
- Inclusions; e.g Glycogen, Protein; Fat globules; Pigments, Crystals
- Organelles
Functions of different cellular structures
| Name of structure | Function |
| Cell membrane | -It forms the boundary of cell -It limits the protoplasmic contents within the cell -It controls the passage of all substances into or out of the cell. |
| Centrosome | -Helps in the process of cell division Give rise to motile cilia or flagella |
| Chromosome | -Determine the sex of offspring. -Carry genetic information from parent to off spring. -Control development and function of cell. |
| Cilia | Defensive activities |
| DNA (Deoxyribonucleic acid) | Bears genetic character Takes part in cell division Take parts in protein synthesis |
| Flagella | Flagella is concerned with movement |
| Golgi complex | -Condensation and packing of secretory products -Active in Lysosome production -Helps in synthesis of glycoprotein -Association with transmission of secretory products |
| Lysosomes | -They act as digestive apparatus -Responsible for cell destruction ( so it is called suicidal bag) -Act as an intra cellular scavenger |
| Microfilaments | -Participate in muscular contraction -Helps in forming skeletal framework of the cell |
| Microtubules | -They form the exoskeleton with microfilament -Provide support and shape of cell |
| Mitochondria | -It is responsible for ATP production, which is the source of energy. So it is called power house of cell. |
| Nucleus | -It is responsible for ATP production, which is the source of energy. So it is called the power house of the cell. |
| Peroxisomes | Contain several enzyme |
| Ribosome | Synthesize protein |
| RNA (Ribonucleic acid) | -Transport coded message from chromosome to chromosome -Transfer activated amino acids -Associated with binding of enzyme for synthesis of peptide bond. |
| Smooth ER | -Associate with CHO metabolism -Synthesis of Lipid |
| Rough ER | -Protein synthesis -Provides a system for transport of newly synthesis protein |
CELL DIVISION
Cell division is a continuous series of complex events by which cells increase in number from preexisting cell.
Types
1. Amitosis: it is a simple and rapid process of cell division where two daughter cells are formed from a parent cell. This type of cell division restricted in pathological condition of cells (tumour cell).
2. Mitosis: it is the most common process of cell division whereby a somatic cell divides to form two daughter cells.
3. Meiosis: Special type of cell division that yield haploid daughter cell from a diploid parent cell. It occurred only in sex cells.
CELLULAR AGEING
Cellular ageing can be defined as the progressive decline in the resistance to stress and other cellular damages, causing a gradual loss of cellular functions and resulting eventually in cell death.
Process of cell ageing
Recent concepts centre on two interrelated processes-
1. The existence of genetically determined clock (i.e. clock gene) that times aging.
2. Effects of continuous exposure to exogenous influences that results in the progressive
accumulation of cellular and molecular damage.
Changes in cell ageing
alterations of aging cell are as follows
Functional
✓ Reduced mitochondrial oxygen utilization
✓ Less synthesis of RNA and DNA
✓ Less capability for repair
✓ As a whole reduction of cell activity
Morphological
✓ Abnormally lobed nuclei
✓ Pleomorphic vacuolated mitochondria
✓ Decreased endoplasmic reticulum
✓ Golgi apparatus
CELLULAR DEATH
In General Pathology Cell death is the biochemical event of a cell ceasing to carry out its functions. This may be the result of the natural process of old cells dying and by external injurious stimulus.
Types of cell death
There are two types of cell death
1. Normal programmed cell death: after completing life span.
2. Abnormal cell death: due to cell injury.
Cellular changes in death
Biochemical events lead to characteristic morphological changes of cell and causes death. Changes depend on type of death.
Fig : Normal cell death
Fig : Abnormal cell death
General changes in cell death may include
- Nuclear fragmentation
- Chromatin condensation
- Chromosomal DNA fragmentation.
- Cell swelling
- Destruction of cytoplasmic contents.
- Blebbing or budding
- Cell shrinkage or become fragmented
Lysosomal activity play a vital role in cell death. Lysosome lyse the cytoplasmic contents. Lysosomal activity is triggered by genetic or chemical stimulus.
After complete death of cell it shredded out or phagocyted. Normal cell death does not initiate any other response. But usually abnormal death initiate inflammation.
CELLULAR RESPONSE
Cell morphology and functions are to maintain homeostasis but are within range. As a result cells always are not able to maintain its morphologic and functional entity. In presence of some stressful and injurious stimuli these entity may become disrupted.
Response of cell to stressful and injurious stimuli is known as cellular response. This phenomenon also known as cellular changes. Cellular response lead to structural and functional change of cell. It may be reversible or irreversible
Stressful and injurious stimulus
Example of some stressful and injurious stimulus are
- Lack of oxygen supply
- Hormonal, enzymatic excess or lacking.
- Nutritional Imbalances; Deficiency or excess.
- Metabolic disorders.
- Immunologic reactions.
- Genetic Defects
- Biological Aging.
- Microorganisms: Bacteria, viruses, fungi, protozoa, helminths etc.
- Trauma.
- Physical agents; e.g. burn. ionizing radiation, cold etc.
- Chemical agents; e.g. poisons, arsenic, lead etc.
Classification of cellular response
The cellular response or cellular changes can be classifies as
- Cellular adaptation
- Atrophy
- Hypertrophy
- Hyperplasia
- Metaplasia
- Cell injury
- Acute
- Reversible or Degeneration
• Cellular swelling
• Fatty changes
- Irreversible
- Necrosis
- Apoptosis
- Subcellular alteration in sub lethal chronic injury
- Intracellular accumulation
- Pathologic calcification
- Irreversible degeneration
- Cell aging
- Neoplasia
Based on reversibility cellular responses can be classified as
| Reversible | Irreversible |
| Cellular adaptation | Irreversible cell injury |
| Reversible Cell injury | Intracellular accumulation |
| Pathologic calcification | |
| Irreversible degeneration | |
| Cell aging | |
| Neoplasia |
Figure: Cellular Response
Cellular response to stimulus
Common example of specific cellular response to different stimulus
| Injurious stimulus | Cellular response |
| Altered physiological stimuli; some nonlethal injurious stimuli ✓ Increased demand, ✓ increased stimulation (e.g., by hormones) ✓decreased nutrients, ✓chronic irritation (physical or chemical) | Cellular adaptations |
| Reduced oxygen supply; chemical injury; microbial infection | Cell Injury |
| Metabolic alterations, chronic injury | ✓ Intracellular accumulations ✓calcification |
| Cumulative sublethal injury over long life span | Cellular aging |
CELLULAR ADAPTATION
In General Pathology Cellular adaptation refers to reversible changes made by a cell in response to adverse environmental changes.
Cellular adaptation is the state of cell between a normal unstressed cell and the overstressed injured cell.
The adaptation may be physiological (normal) Or pathological (abnormal).
Changes in cellular adaptation
Common adaptation changes in the
✓ Size
✓ Number
✓ Phenotype
✓ Metabolic activity
✓ Functions, etc.
Classification
Cellular adaptation can be classified as
1. Atrophy
2. Hypertrophy
3. Hyperplasia
4. Metaplasia
5. Dysplasia
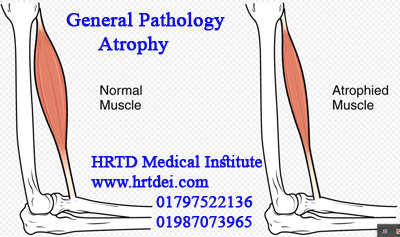
ATROPHY
Atrophy means shrinkage of in the cell size due to loss of cell constituents. The term ‘Atrophied’ means atrophy takes place.
When sufficient number of cells become atrophied the size of organ or tissue become diminished.
Causes of atrophy In General Pathology
Common causes of atrophy
- Decreased work load.
- Loss of innervation.
- Diminished blood supply.
- Inadequate nutrition.
- Loss of endocrine stimulation.
- Aging.
- Pressure.
Classification
Atrophy can be classified as
Physiological
- At fetus life: atrophy of bronchial cleft, notochord, thyroglossal duct.
- At Infancy: atrophy of ductus arteriosus, umbilical vessels.
- At Puberty: atrophy of lymphoid tissue, thymus.
- At old age: atrophy of reproductive organs.
Pathological
Generalized
- Starvation atrophy; e.g. kwashiorkor.
- Senile atrophy (at old age).
- Endocrine atrophy; e.g. in hypopituitarism.
Figure: Normal & Atrophied cell and organ
Localized
- Ischaemic atrophy; e.g. cerebral arterial atheroma.
- Pressure atrophy; e.g. capsular cells of benign tumour.
- Disuse atrophy; e.g. atrophy of related muscles, ligaments when the bone is immobilized.
- Neuropathic atrophy; e.g. wasting of limb in lower motor neurone disease, poliomyelitis.
- Idiopathic; e.g. idiopathic myopathy.
HYPERTROPHY In General Pathology
Hypertrophy is the increase in size of organ due to enlargement of cell resulting from increase in cellular constituents (e.g. myo filaments). The term ‘Hypertrophied’ means hypertrophy takes place.
Causes of hypertrophy
General causes of hypertrophy
✓ Increased Functional demand
✓ Specific hormonal stimulation
Site of hypertrophy
Common site of hypertrophy is muscle. Generally it is found in
✓ Skeletal muscle
✓ Cardiac muscle
✓ Uterine muscle
✓ Smooth muscles of GIT
Types of hypertrophy
(a) Physiological hypertrophy: It is a normal phenomenon; e.g. uterus in pregnancy, hypertrophy of breast during lactating, muscles of athletes, etc.
(b) Adaptive hypertrophy. Occurs due to increased work load; e.g. Hypertrophy of left ventricle in hypertension, if ant one kidney is removed then another kidney shows hypertrophy.
(c) Pathological hypertrophy; e.g. cells of strictures: such as urethral, oesophageal stricture, intestinal stricture in TB, pyloric stenosis etc.
Figure: Hypertrophy
METAPLASIA In General Pathology
Metaplasia is a reversible change of tissue in which one cell type is replaced by another cell type.
As a result of metaplasia one type of epithelium is changes to another type (e.g. columnar to stratified squamous). Similarly one type of connective tissue transformed to another type of connective tissue (e.g. fibroblast to bone).
Metaplastic tissue better able to withstand adverse environment.
Because protective activity of the tissue is increased due to metaplastic change.
Metaplasia serves as subsoil for subsequent cancer transformation if the influences are persistent and continuous.
Principal cause metaplasia is chronic irritation.
Types of metaplasia
Broadly metaplasia can be classified as
1) Epithelial metaplasia
- Squamous metaplasia: Commonly found. Many types of epithelium are capable of changing to a stratified squamous epithelium due to persistent injurious effect (ch. irritation) e.g.
- Trachea & bronchi: in cigarette smoker & chronic bronchitis. Here ciliated columnar epithelium is replaced by stratified squamous.
- Gall bladder: in chronic cholecystitis & cholelithiasis. Here tall columnar is replaced by stratified squamous.
- Kidney & bladder: in stone and chronic infection. Here transitional epithelium is replaced by strati. fied squamous.
- Uterus: the cervix frequently undergoes squamous metaplasia in chronic cervicitis.
- Columnar metaplasia: Here Squamous types of epithelium transformed to columnar epithelium. e.g.
- Vaginal cervix: metaplasia in cervical erosion.
- Oesophagus: metaplasia as a result of chronic acid reflux into oesophagus.
- Stomach: metaplasia in the stomach associated with chronic gastric ulcer.
Figure: Metaplasia
2) Connective tissue metaplasia
- Osseous metaplasia: injury to soft tissue causes fibroblast formation and fibroblast may transform to osteoblast (a cell of bone). e.g. dystrophic calcification in scar,Myositis Ossificans.
- Due to aging costal and hyaline cartilage may transformed to bone.
3) Tumor metaplasia
It means metaplasia in tumour cells. The occurrence of mixed adeno carcinoma & squamous cell carcinoma (adenoacanthoma) may be explained on the basis of tumour metaplasia. Tumour metaplasia of squamous type seen in
✓Squamous cell carcinoma of the lung.
✓ Carcinoma of the gall bladder.
✓Endometrial adenocarcinoma.
✓ Transitional cell carcinoma of urinary tract.
4) Mucoid metaplasia
Here normal cell replaced by mucin secreting cell. Occasionally seen in
✓ Adenocarcinomata of the breast.
✓Otitis media
DYSPLASIA In General Pathology
Dysplasia may be defined as non neoplastic proliferative disorder where atypical cytological alteration in size, shape and organization is seen.
Dysplastic changes are always reversible. Removal of causative stimuli cells converted to normal. But if stimuli are persist then dysplastic change may transform to cancer.
Principal cause of dysplasia is chronic irritation or inflammation.
Histological characteristic of dysplasia
- Variation in cell size and shape
- Atypical proliferation
- Large and darkly stained nuclei
- Mitosis
Sites
Dysplasia can be found
Common
✓Cervix in chronic cervicitis
✓ Reparatory tract in chronic cigarette
✓ Skin
✓ urinary bladder
✓ Larynx
Uncommon
- Oral mucosa
- Gall bladder
- Bone marrow
Figure: Dysplasia
CELL INJURY In General Pathology
Cell injury
It is a state of a cell where its homeostasis is not maintained and the cell may become functionally impaired.
Causes of Cell Injury
General causes of cell injury can be summarized as-
- Lack of oxygen supply
- Ischaemia: due to diminished arterial flow or reduced venous drainage, (eg. in atherosclerosis, thrombosis, embolism etc.)
- Inadequate oxygen carrying capacity of blood, (eg. in anaemia, carbon monoxide poisoning etc.)
- Hypoxia: due to inadequate oxygenation of blood in cardiac failure, respiratory failure etc.
- Microorganisms: Bacteria, viruses, fungi, protozoa, helminths etc.
- Trauma.
- Physical agents; e.g. burn. ionizing radiation, cold etc.
- Chemical agents; e.g. Alcohol, cytotoxic drugs, poisons etc.
- Immunologic reactions; e.g. hypersensitivity.
- Nutritional Imbalances; eg. protein energy malnutrition, vitamin deficiency.
- Metabolic disorder
- Genetic Defects
- Aging.
Lack of oxygen supply
The lack of oxygen causes the aerobic pathways of respiration to cease. As a result the mitochondrial electron transport of oxidative phosphorylation stops. This causes the level of cellular ATP to decrease.
Decreased ATP level causes the stoppage of the sodium- potassium pump. This creates an imbalance of ions, which causes the cell to disrupt the intracellular environment.
This decreased ATP level also leads to the breakdown of the Thus cellular pH decreased. pyruvate formed by glycolysis into lactate and then lactic acidosis.
Decreased pH increase cell membrane permeability and also damages the lysosomal membranes. Damage of lysosomal membrane causes internal
digestion of cell contents and finally destruction of cell.
Mechanical trauma In General Pathology
In General Pathology Mechanical trauma may cause subtle but significant dislocations by completely disrupting it.
Physical agents
Low temperature
- Induces vasoconstrictions & impairs blood supply to cells.
- In case of persistence injury, it leads to disturbance of vasomotor control. It causes marked vasodilatation lead to intravascular coagulation. As a result impairment of blood supply takes place.
- When temperature becomes sufficiently low, intracellular water crystallizes.
Burn or extreme temperature
- Direct coagulation of protein leads to cell damage.
High temperature
- Lead to hypermetabolism and causes accumulation of acid metabolites and lowering pH.
Sudden changes in atmospheric pressure
- Lead to impairment of blood supply to cells.
Electric energy
- Produce heat →bum.
- It may interfere with neural conduction pathways
Radiation
- Direct Ionization of chemical compounds contained within the cell
- Ionization of cellular water producing free hot radicals that secondarily interact with intracellular constituents
- Induces varying mutations that may injure & even kill cells.
Microbiological agents
Possible mechanism are-
- Toxin: damage different cellular parts.
- Enzyme: damage different cellular parts.
- Direct effect: e.g. virus infection. Replication within cell and causes metabolic disorder of the cell.
- Chromosomal change: by virus
- Hypersensitivity reaction
- Mechanical presence; e.g. Wuchereria bancrofti lymphatic obstruction.
- Rubbing of nutrition of host; e.g. intestinal worm.
Chemicals agents
- Direct effect on cellular component, e.g. denaturation of protein.
- Causes cell membrane permeability.
- Formation of free radicals: interfere chemical reactions within cell and causes disorder.
Immunologic reactions
- Different types of immunological reaction can cause cellular damage (mainly by phagocytosis mechanism).
Nutritional Imbalances
- Deficiency of nutrients interfere cellular metabolism and causes cell injury.
Metabolic disorder
- Impaired metabolism or hyper metabolism lead to cell injury.
Genetic Defects
- Leads to morphological and functional defect of cell
Aging
- Leads to morphological and functional defect of cell
Classification of Cell Injury In General Pathology
In General Pathology Cell injury cab be classified as
a) Reversible cell injury (also known as degeneration)
1. Cellular swelling
2. Fatty changes
b) Irreversible cell injury
1. Necrosis
2. Apoptosis
REVERSIBLE CELL INJURY
Reversible cell injury or Degeneration
Reversible cell injury or Degeneration can be defined reversible cellular morphological changes resulting from lethal injury.
Cause
Mainly due to metabolic defect.
Cellular changes in degeneration
Basic change in degeneration
- Morphological change of organelles
- Appearance of extra components e.g. vacuoles, granules etc.
- Nucleus normal.
Classification
Reversible cell injury or Degeneration can be classified as-
1. Cellular swelling
2. Fatty changes
CELLULAR SWELLING In General Pathology
In General Pathology, Cellular swelling can be defined as a condition of cell when it is not capable for maintaining ionic and fluid homeostasis result in accumulation of excess fluid into cell. Also known as hydropic change or vacuolar degeneration or cloudy swelling.
Causes of cellular swelling
Common causes include-
✓ Lack of oxygen supply, Ischemia, hypoxia etc.
✓ Bacterial toxin
✓ Chemicals; e.g. carbon tetra chloride, chloroform etc.
✓ Burn
✓ High fever
✓ Hypokalemia
Organ involved
Cellular swelling commonly found in
- Liver
- Kidney
- Heart
Changes in cellular swelling
Macroscopic appearance:
- The organ is enlarged, swollen, pale, and increased in weight.
- Soft in consistency
- The cut surface bulges outwards
Microscopic appearance
- Cells are enlarged and swollen
- Cytoplasm is granular
- Compression of microvasculature of organ e.g. hepatic sinusoids and capillary network within the renal cortex
- Sometimes, the appearance of small clean vacuoles within the cytoplasm.
- Nucleus normal
Figure: Cellular swelling
FATTY CHANGES In General Pathology
In General Pathology, The term fatty change refers to the abnormal accumulation of triglycerides within parenchymal cells. Also known as Steatosis or fatty degeneration or adipose degeneration.
Causes of fatty changes
Nutritional
- Kwashiorkor
- Obesity
Metabolic disease
- Type II diabetes mellitus
- Galactosaemia
- Glycogenosis
- Hyperlipedemia. Etc
Drug & chemicals
- Alcohol
- Corticosteroid
- High dose estrogen.
- Hepatotoxic substances. etc
Others
- Any pathology that causes vascular ischemia.
- Viral infection
- Bacterial toxin (e.g. diphtheria)
- Pregnancy (liver involved)
- Systemic disease
- Pancreatic disease
- Gastrointestinal disease
- Sleep apnoea
Organs involved
✓ Liver (most found)
✓ Heart
✓ Kidney (mostly in tubular epithelium)
✓ Pancreas. etc
Changes in fatty change
Macroscopic
- Organ may enlarged (liver).
- Weight gain of organ (liver).
- Change in color
- May become soft & flabby
- The cut surface may show a greasy appearance (kidney)
Microscopic
- The appearance of small fat vacuoles within the cytoplasm
- Nucleus normal.
Figure: Fatty changes
IRREVERSIBLE CELL INJURY In General Pathology
In General Pathology, Irreversible cell injury means the morphological changes that follow cell death in a living tissue or organ. The cells cannot come to their original form after the removal of injurious agents.
Classification
Irreversible cell injury is classified as
1. Necrosis
2. Apoptosis
NECROSIS In General Pathology
In General Pathology, Necrosis is the sum of the morphological changes within an injured cell of living tissue that follow cellular death. Here cellular death occurs due to the direct effect of injurious stimulus.
After necrosis inflammation may take place in the tissue.
Pathogenesis of necrosis
There are two events those responsible for necrosis
- Enzymatic digestion of cell.
- Denaturation of protein: after denaturation enzymatic digestion of protein takes place. Denaturation is done by
- Autolysis: It means self destruction. It is done by the catalytic enzymes that are released from lysosomes of lethally injured cells which cause denaturation of protein.
- Heterolysis: It means destruction by others. It is done by the catalytic enzymes that are released from lysosomes of immigrant leukocytes causing denaturation of protein.
Figure: Necrosis
Changes in necrosis
General changes.
✓ Cell swelling
✓Denaturation and coagulation of protein
✓ Breakdown of cellular organelle
✓ Cell rupture
Specific changes
Nuclear changes: may be
1. Pyknosis: Shrinkage of nuclear materials
2. Karyorrhexis: Fragmentation of nuclear materials
3. Karyolysis: Breakdown of nuclear materials
Cytoplasmic changes may be
- Glassy homogenous appearance due to loss of glycogen.
- Moth eaten appearance (cytoplasm vacuolated)
- Eosinophilia – (loss of basophilia due to loss of RNA, denatured protein).
- Overt discontinuities in plasma and organelles membrane.
- Dilation of mitochondria with densities (appearance of myelin figure)
- Fluffy material of denatured protein
Eosinophilia: ability to take up ‘Eosin stain’.
Basophilia: ability to take up ‘Basic stain (e.g. hematoxylin)’
Classification of Necrosis
Basic types
- Coagulative necrosis
- Liquefactive necrosis
Special types
1. Caseous necrosis
2. Fat necrosis
- Enzymatic necrosis
- Traumatic necrosis
3. Gangrenous necrosis
4. Fibrinoid necrosis
5. Gummatous necrosis
6. Necrosis of muscles
COAGULATIVE NECROSIS In General Pathology
In General Pathology, Coagulative necrosis is the most common pattern of necrosis and is characterized by the conversion of the cell to an acidophilic opaque mass.
cause of coagulative necrosis is hypoxia.
Figure: Coagulative necrosis in kidney and heart
Features
- Coagulation of protein is superimposed than enzym digestion.
- Usually occurs with loss of the nucleus
- Preservation of the outline of the cell
- Denaturation of both structural and enzymatic protein
Site of coagulative necrosis
Common site of coagulative necrosis
- Heart (myocardial infarction)
- Kidney
- Liver
- Adrenal gland.
LIQUEFACTIVE NECROSIS In General Pathology
In General Pathology, Liquefactive necrosis or colliquative necrosis is a type of necrosis characterized by digestion of the dead cells, resulting in transformation of the tissue into a liquid viscous mass. Often it is associated with microbial (e.g. bacteria) infection.
Features
- Enzymatic digestion is more than protein digestion.
- Autolysis & heterolysis prevail over protein denaturation.
- No architecture of cell
- Necrotic area soft & filled with fluid.
- Accumulation of acute inflammatory cell (neutrophil) near the injured/death cell.
Common sites
✓ Bacterial infection (pyogenic abscess- most common).
✓ Hypoxic death of the cells of CNS
Figure: Liquefactive necrosis
CASEOUS NECROSIS
It is a special type of necrosis where the tissue shows cream. cheesy (caseous) appearance.
Morphology
- Gross features: soft, granular, and friable as cream -cheesy (caseous) appearance.
- Light Microscopy: Granular and eosinophilic. Architecture of cell is completely destroyed. Granuloma is formed with central cheesy material rimmed by epitheloid cells & giant cells (foreign body giant cells/Langhans giant cells). Tuberculosis coagulative necrosis is modified by capsule of lipopolysaccharide of Tb bacilli.
Examples
It is seen in Tuberculosis (most common), syphilis, and some fungal infections.
FAT NECROSIS
Fat necrosis is a special type of necrosis when fat cells are involved.
In fat necrosis, the enzyme lipase releases fatty acids from triglycerides. The fatty acids then complex with calcium to form soaps as white chalky material.
Figure: Fat Necrosis
Morphology
Gross: Opaque and chalky
Light Microscopy: Shadowy outlines of dead fat cells found. Outline of necrotic fat cells filled with amorphous basophilic erial (calcium soaps). Sometimes there is a bluish cast from to calcium deposits, which are basophilic.
Classification
There are two types of fat necrosis-
- Enzymatic necrosis; is commonly found in pancreas (after pancreatitis).
2. Traumatic necrosis; found in breast tissue (as a result of trauma).
Example
It is found in the Pancreas, Breast tissue and other adipose tissue.
FIBRINOID NECROSIS
Fibrinoid necrosis is a special type of necrosis in which there is an accumulation of amorphous, basic, proteinaceous material in the tissue matrix with staining reactions resembling fibrin.
Commonly in fibrinoid necrosis immune complexes (complexes of antigens and antibodies) combine with fibrin.
Site
Interstitial collagen and blood vessels (small artery and arteriole)
Features
Vessel walls are thickened and show amorphous pink circumferential necrosis with inflammation.
Examples
- In allergic reactive diseases: Rheumatic fever, SLE, polyarteritis nodosa, some collagen disease, hyperacute transplant rejection, etc.
- In non-allergic reactive diseases: malignant hypertension,
- Others: preeclampsia.
Figure: Fibrinoid Necrosis
GUMMATOUS NECROSIS
Necrosis forms a dry rubbery mass (gumma) associated with spirochetal diseases (e.g.syphilis).
Gummatous necrosis is thought to be a hypersensitivity reaction directed against spirochetes.
Characteristics
- Gross: firm and rubbery appearance.
- Microscopy: they do not have complete obliteration of cellular architecture. Gummas are surrounded by a rim of fibroblasts, macrophages, lymphocytes, plasma cells, and occasional multinucleated giant cells. Treponemas arc is rarely identified in the tissue.
Site
Skin and bone are the most common sites. Also found in the liver (called hepar lobatum), brain, testis, heart, and other soft tissue.
Figure: Gummatous necrosis on the skin (in syphilis)
NECROSIS OF MUSCLE
It is a special type of necrosis caused by the progressive degradative action of enzymes that is generally associated with severe cellular trauma in muscles.
Characteristics
- Gross: Muscle fiber cross-sections contain pale & hypercontracted regions.
- Microscopy: Pale cytoplasm staining. Intermyofibrillar network absent. Nuclease is absent or reduced staining. Loss of plasma membrane. Myofibrils are lysed or lost. Lately granular or filamentous debris in fiber.
Site
Muscle trauma site.
Figure: Necrosis of muscle
GANGRENE/GANGRENOUS NECROSIS
In such necrosis ischemic death of cells & coagulative necrosis take place.
In short gangrenous necrosis termed as gangrene.
Gangrene is the necrosis of the tissue followed by putrefaction o desiccation.
Types
According to the characteristics of the invasion area
1. Dry gangrene: where the site becomes desiccated.
2. Moist gangrene: where the site is putrefied.
3. Gas gangrene: gas bubbles are present in the area. Basically, it is a type of moist gangrene.
DRY GANGRENE In General Pathology
In General Pathology, Dry gangrene is the macroscopic death of tissue followed by desiccation. It is a result of ischaemic coagulative necrosis of tissue due to lack of arterial supply.
Causes of dry gangrene
The cause of dry gangrene is due to arterial obstruction. The causes of arterial obstruction are as follows-
- Changes in the arterial wall in Buerger’s disease, arteriosclerosis, and atherosclerosis.
- Spasm of the blood vessels. (e.g. in Raynaud’s disease and ergot poisoning.)
- Obstruction within the lumen due to thrombosis, embolism, and thromboembolism.
- Pressure from outside by tumor, tight plaster, etc.
Features of dry gangrene
- Commonly occurs in the extremities (mainly the lower limb)
- Result from arterial occlusion (partial obstruction).
- The affected part becomes dry, discolored (usually black), and wrinkled.
- The affected area is cold to touch (due to a lack of blood supply).
- The affected area is separated from the healthy part by a sharp line (made of granulation tissue) called a demarcation line
- Usually not associated with infection.
Figure: Dry gangrene on the finger (Buerger disease)
MOIST GANGRENE/ WET GANGRENE
Moist gangrene is the macroscopic death of tissue followed by purification. Moist gangrene develops due to obstruction of both arterial supply and venous drainage.
Features of moist gangrene
- The affected part becomes swollen & discolored (reddish black).
- The area is moist (due to extensive liquefaction of dead tissue).
- A foul smell comes from the site (due to the formation of indole and skatole).
- Bleb or crepitation present.
- There is no line of demarcation.
- Infection is always present
Common sites
The common sites of moist gangrene
✓ Bed sores
✓ Mouth
✓ Intestine
✓ Lungs
✓ Abdominal wall
✓ Vulva
✓ Cervix of uterus
✓ Scrotum
✓ Thigh
✓ Extremities.
Figure: Moist gangrene
GAS GANGRENE In General Pathology
In General Pathology, Gas gangrene is a type of moist gangrene caused by some anaerobic bacteria belonging to the genus Clostridia where gas bubbles are found in affected area.
Common sites
- Deep wounds e.g. gunshot, lacerated wound, penetrating wound etc.
- Wound heavily contaminated with soil or animal feces.
- Compound fracture.
Causative bacteria
Saccharolytic Clostridia
- CI. welchii
- CI. Oedematiens
- CI. septicum
Proteolytic Clostridia
- CI. histolyticum
- CI. sporogenes
Figure: Gas gangrene
Features of gas gangrene
- Usually manifests within 24-72 hours of injury.
- The affected part becomes markedly swollen.
- The overlying skin becomes tense (due to internal pressure).
- Muscles become discolored (brick red), soft, and friable.
- The foul smell comes from the site.
- Discharges contain gas bubbles.
- Bleb or crepitation present.
DIFFERENCE BETWEEN DRY AND MOIST GANGRENE
| Point | Dry gangrene | Moist gangrene |
| Cause | Due to arterial obstruction | Due to arterial & venous obstruction |
| Type of arteria obstruction | Partial | Complete |
| Area | The area is dry | The area is moist |
| Foul smell | Absence | Present |
| Bleb or crepitation | Absent | Present |
| Line of demarkation | Present | Absent or indistinct |
| Putrefaction | No putrefaction | Very rapid putrification. |
| Spread | Slow spread. | Rapid spread |
| Infection | Usually not associated | Commonly associated |
| Common sites | Usually occurs in the internal organ | Usually occur in the internal organ |
| Prognosis | Usually not fatal | Usually fatal |
 HRTD Medical Institute
HRTD Medical Institute




