Paramedical Course 4 Years Details
Paramedical Course 4 Years : Mobile Number. 01987073965, 01941123488, 01797522136. A Paramedical course of 4 years duration is a Long type of Paramedical Course in Bangladesh. This Course contains 30 subject in 8 semesters. The 1st semester contains 5 subject and 2nd semester contains 5 subjects. 3’rd semester contains 4 subjects & 4th semester contains 4 subjects. 5th semester contains 3 subject & 6th semester contains 3 subjects. 7th semester contains 3 subject & 8 semester contains 3 subjects.

Paramedical Course 4 Years are available in HRTD Medical Institute. This Institute is an Organization of HRTD Limited ( Registered by the Govt of the People Republic of Bangladesh).
Location of Paramedical Course 4 Years
Location of Paramedical course 4 Years Training center. Mobile no. 01987073965, 01941123488, 01797522136. HRTD Medical Institute, Abdul Ali Madbor Mansion, Section-6, Block-Kha, Road-1, Plot-11, Mirpur-10 (Gol-Chattar) Metro Rail Piller No-249, Dhaka-1216.
Course Fee for Paramedical Course 4 Years in Dhaka, Bangladesh
Course Fee for Paramedical Course 4 Years. Mobile No. 01987073965, 01797522136. Paramedical Course Fee for 4 Years TK 1,82,500/- Including Admission Fee, Monthly Fee & Exam Fee.
Paramedical Course 4 Years Admission Eligibility
Paramedical Course Admission Eligibility. Mobile No. 01987073965, 01797522136. SSC or Equivalent/ HSC/ Degree/Master’s from Any Background (Science/ Arts/ Commerce/ Technical).
Hostel Facilities in HRTD Medical Institute for Paramedical Course 4 Years
Hostal & Meal Facilities
The Institute has hostel facilities for the students. Students can take a bed in the hostel.
Hostel Fee Tk 3000/- Per Month
Meal Charges Tk 3000/- Per Month. ( Approximately )
হোস্টাল ও খাবার সুবিধা
ইনস্টিটিউটে শিক্ষার্থীদের জন্য হোস্টেল সুবিধা রয়েছে। ছাত্ররা হোস্টেলে বিছানা নিতে পারে।
হোস্টেল ফি 3000/- টাকা প্রতি মাসে,
খাবারের চার্জ 3000/- টাকা প্রতি মাসে।(প্রায়)
Address of HRTD Medical Institute for Paramedical Course 4 Years
আমাদের ঠিকানাঃ HRTD মেডিকেল ইন্সটিটিউট, আব্দুল আলী মাদবর ম্যানশন, সেকশন ৬, ব্লোক খ, রোড ১, প্লট ১১, মেট্রোরেল পিলার নাম্বার ২৪৯, ফলপট্টি মসজিদ গলি, মিরপুর ১০ গোলচত্ত্বর, ঢাকা ১২১৬ । মোবাইল ফোন নাম্বার ০১৭৯৭৫২২১৩৬, ০১৯৮৭০৭৩৯৬৫ ।
Our Address: HRTD Medical Institute, Abdul Ali Madbor Mansion, Section-6, Block- Kha, Road- 1, Plot- 11, Metro Rail Pilar No. 249, Falpatty Mosjid Goli, Mirpur-10 Golchattar, Dhaka 1216. Mobile Phone No. 01797522136, 01987073965.
Why a Paramedical Course 4 Years is Essential in Bangladesh
A four-year paramedical course is essential in Bangladesh because it provides the in-depth knowledge and advanced practical skills needed to address the country’s growing healthcare demands and improve the quality of healthcare services. While shorter diploma programs exist, a longer course equips paramedical professionals with the proficiency to handle a wider range of complex medical scenarios, ensuring better patient outcomes and supporting physicians in delivering comprehensive and efficient care.
Key Reasons for a 4-Year Course:
- Enhanced Skill and Knowledge:A longer duration allows for more in-depth theoretical learning and extensive hands-on training in various practical skills.
- Improved Quality of Care:With better-trained professionals, the overall standard of healthcare services in Bangladesh can be significantly elevated.
- Addressing Complex Needs:A four-year program prepares professionals to handle a wider range of medical situations and complexities, which is crucial for a rapidly developing nation’s healthcare system.
- Critical Role in the Healthcare System:Paramedical professionals form the backbone of the healthcare industry, and extended training ensures they can provide more efficient and effective support to physicians and patients.
- Specialization and Expertise:A longer course enables students to develop greater expertise and potentially specialize in specific areas of paramedical care, further enhancing the efficiency of healthcare delivery.
- Alignment with International Standards:Longer and more comprehensive paramedical education aligns with the standards in developed countries, raising the benchmark for healthcare professionals in Bangladesh.
- Meeting Demand:As the healthcare industry expands, there is a growing demand for highly qualified paramedical staff to fill crucial roles and maintain a robust healthcare infrastructure.
Some Subject for Paramedical Course 4 Years In Dhaka, Bangladesh
Paramedical Course subjects. Mobile No. 01987073965, 01797522136.
- Human Anatomy & Physiology-1
- Pharmacology-1
- Study of OTC Drugs
- First Aid-1 & 2
- Practice of Medicine
- Hematology
- Pathology for Medical Practice
- General Surgery-1
- Cardiovascular Anatomy
- Antimicrobial drugs
- Medical Diagnosis-1 & 2
- Chemistry
- Medical Biochemistry
- Orthopedic Anatomy
- Neuro Anatomy & Physiology
- Pharmacology-2
- Pathology- 1 & 2
- Anatomy & Physiology-2
- Respiratory Disease & Treatment
- Essential Drugs & Medicine
- Human Microbiology
- Community Medicine-1&2
- ENT Drugs & Ophthalmic Drugs
- Urology & Hepatology
- Fungal Infections and Treatment
- Medical Diagnosis & Treatment
- Common Respiratory Disease
- Cardiovascular Drug & Disease
- Practice of Neuromedicine
- Abdominal Pain Management
Practical Classes And Internship for Paramedical Course 4 Years
Heartbeat, Heart Rate, Cardiac Auscultation, Process of Cardiac Auscultation, Tachycardia, Bradycardia, Pulse, Pulse Rate, Strong Pulse, Weak Pulse, Blood Pressure, Normal Blood Pressure, Systolic Blood Pressure, Diastolic Blood Pressure, Pulse Pressure, Mean Blood Pressure, Hypertension, Hypotension, Hypertension Emergency, First Aid and Management of Hypertension Emergency, Cleaning, Dressing, Bandaging, Stitching, Inhaler, Rotahaler, Nebulizer, Pulse Oxymter, Oxygen Cyllinder, Injection Pushing, IM Injection Pushing, IV Injection Pushing, SC Injection Pushing, Vaccine Pushing, Insulin Pushing, Blood Glucose Masurement, Diabetes, Saline Pushing, Respiratory Meter, First Aid and Management of Shock, First Aid of Bone Fracture, X Ray Report Understanding, Respiration, Respiratory Auscultation, Process of Respiratory Auscultation, First Aid of Diarrhea and Constipation, Dehydration Test, Edema Test, Joundice Test, Anemia Test, etc.
Teachers For Paramedical Course 4 Years
Dr. Sakulur Rahman (MBBS,CCD)
Dr. Tisha (MBBS)
Dr. Sanjana Ahmed (BDS)
Dr. Disha (FCPS)
Dr. Kazi Mahinul (MBBS)
Dr. Najmun Nahar Juthi (BDS)
Dr. Md. Niamul (MBBS)
Dr. Kamrunnahar Keya (BDS)
Dr. Suhana (MBBS, PGT)
Dr. Shamima (MBBS,PGT)
Dr.Layla (MBBS)
Dr. Farabi (MBBS)
Dr.Nurunnahar (BDS)
Dr.Rajoan (MBBS)
Human Anatomy & Physiology For Paramedical Course 4 Years
The Study of the body Structure and its function is Anatomy & Physiology. Here we discuss the systems of the human body and its organ, Tissues, and cells. The systems of the human body are the digestive system, Respiratory system, Cardiovascular system, Skeletal system, Muscular system, nervous system, Endocrine system, Immune System, Integumentary System and Urinary System.
Human Anatomy and Physiology is the study of the body’s structures (anatomy) and their functions (physiology). Anatomy focuses on the physical arrangement of cells, tissues, organs, and systems, while physiology explains how these structures work together to maintain life processes like movement, metabolism, and reproduction. The two are intertwined, as a structure’s form determines its function, and understanding one requires understanding the other.
Anatomy
- Definition:The scientific study of the body’s structures and their physical arrangement.
- Levels of Study:Can be studied at different levels, including:
- Gross Anatomy: The study of structures visible without a microscope, such as organs and organ systems.
- Microscopic Anatomy (Histology): The study of tissues and cells using a microscope.
- Methods of Study:Historically involved dissection, but now also uses advanced imaging techniques like MRI and CT scans to visualize structures in living people.
Physiology
- Definition: The study of how the body’s structures function to sustain life.
- Key Concepts:
- Complementarity of Structure and Function: The shape and form of a body structure are directly related to what it can do.
- Homeostasis: The body’s ability to maintain a stable internal environment, which is essential for survival.
- Examples: Studying how the heart regulates blood flow or how muscles contract and bring bones together.
Major Body Systems
Understanding human anatomy and physiology involves studying the body’s major systems, including:
Musculoskeletal System, Circulatory System, Nervous System, Digestive System, Respiratory System, Integumentary System, Endocrine System, Lymphatic System, Urinary System, and Reproductive System.
Why It’s Important
- Health Professions:It is a fundamental science for careers in medicine and other health fields.
- Personal Health:Knowledge of the human body helps in making informed health decisions and understanding medical information.
Pharmacology-1 for Paramedical Course 4 Years
The study of drugs and Medicine is called Pharmacology. Here we discuss group-wise drugs and their medicines in Pharmacology-1. Common Group of Drugs are pain killer drugs, Anti ulcer Drugs, Anti Vomiting Drugs, Laxative Drugs, Motility Drugs, Antimotility Drugs, Bronchodilator Drugs, Antibiotic Drugs. Anti Fungal Drugs, Anti Protozoal Drugs, Anti Viral Drugs, Anthelmintic Drugs, Anti Hypertensive Drugs, Beta Blocker Drugs, Calcium Channel Blocker Drugs, Antipyretic Drugs, Anti Thrombotic Drugs etc.
First Aid for Paramedical Course 4 Years
First Aid is an important subject for Medical courses including Diplomas in Medicine & Surgery course. RMP Courses, LMAF Courses, Paramedical Courses, DMA Courses, DMS Courses, Nursing Courses, Dental Courses, Pathology Courses, Physiotherapy Courses, Caregiver courses etc. Here we discuss shock, Classification Shock, causes of Shock, Stages of Shock, Clinicle Features of Shock, Hypovolemic Shock, Cardiogenic Shock, Neurogenic Shock, Traumatic Shock, Burn Shock, Electric Shock, Psychogenic Shock, Anaphylactic Shock, First Aid of Shock, First Aid of cut, First Aid of Snake Bite, First Aid of Accidental Injury etc.
Study of OTC Drugs for Paramedical Course 4 Years
OTC Drugs are important for all Medical Assistant Courses, Diploma Medical Courses, LMAF Courses and RMP Courses. It is also important for the Diploma in Medicine & Diploma in Surgery Course. These OTC Drugs can be sold purchases without any prescription From Registered MBBS Doctors. These Drugs are Emergency and safe for the patients. The Study of OTC Drugs improves the quality of practice. Some OTC Drugs are Albendazole, Ascorbic Acid, Calcium, Multivitamins, Vitamin B Complex, Omeprazole, Oral Rehydration Salt, Salbutamol etc.
Respiratory Disease for Paramedical Course 4 Years
1. Diagnosis and Monitoring:
- Early Detection: AI algorithms can analyze medical images (X-rays, CT scans) and respiratory sounds to detect conditions like lung cancer, COPD, and asthma earlier than traditional methods.
- Improved Accuracy: AI can assist radiologists in classifying normal and pathological radiographs with increased accuracy, reducing reporting time and potential errors, according to Archivos de Bronconeumología.
- Personalized Monitoring: AI-powered devices can monitor lung function at home, providing real-time feedback to patients and enabling remote monitoring of disease progression.
- Respiratory Sound Analysis:AI algorithms can analyze nasal and oral breathing sounds to detect respiratory conditions, providing a non-invasive and convenient diagnostic tool.
2. Treatment Optimization:
- Personalized Medicine:AI can analyze patient data (medical history, genetic information, treatment response) to predict the best treatment approach for individual patients, optimizing treatment outcomes and minimizing side effects.
- Ventilator Management:AI can analyze patient data in real-time to optimize ventilator settings for patients on mechanical ventilation, ensuring optimal lung function and minimizing complications.
3. AI in Clinical Trials:
- Efficient Data Collection: AI can improve the quality of data collected in clinical trials by providing real-time feedback to patients during spirometry tests and automating the process of reviewing and assessing data.
4. Key AI Applications:
- Lung Cancer Screening:AI can be used to analyze CT scans for lung cancer, identifying nodules and predicting the risk of malignancy.
- COPD and Asthma Management:AI algorithms can assist in the early detection and personalized management of COPD and asthma.
- Infectious Disease Diagnosis:AI can analyze respiratory sounds and images to diagnose respiratory infections like pneumonia and COVID-19.
5. Challenges and Ethical Considerations:
- Data Privacy and Security:Protecting patient data and ensuring the responsible use of AI algorithms is crucial.
- Bias and Fairness:Ensuring AI algorithms are free from bias and that they provide equitable care for all patients is essential.
- Transparency and Explainability:Understanding how AI algorithms make decisions is important for building trust and ensuring accountability.
Orthopedic Anatomy For Paramedical Course 4 Years
Important topics in orthopedic anatomy include the skeletal system (bones, joints, and their articulations), muscles, tendons, ligaments, and nerves. Understanding these structures, their interactions, and common injuries like fractures, dislocations, and soft tissue damage is crucial. Key areas include the upper limb (shoulder, elbow, wrist, hand), lower limb (hip, knee, ankle, foot), and spine.
Key Areas and Specific Topics:
- Skeletal System:
- Bones: Types of bones (long, short, flat, irregular), bone structure (compact and spongy), bone formation (endochondral and intramembranous ossification), and common fractures.
- Joints: Types of joints (fibrous, cartilaginous, synovial), examples of each (e.g., shoulder, hip, knee, elbow, ankle, wrist).
- Spine: Vertebral column structure (vertebrae, intervertebral discs, facet joints), spinal curves, and common spinal conditions.
- Musculoskeletal System:
- Muscles: Muscle origins, insertions, actions, and innervation, particularly focusing on muscles of the limbs and back.
- Tendons and Ligaments: Their roles in joint stability and common injuries (e.g., tendonitis, ligament sprains).
- Nerves: Major nerves in the limbs (e.g., radial, ulnar, median, sciatic, femoral), nerve injuries (e.g., carpal tunnel syndrome, sciatic nerve compression), and their impact on movement and sensation.
- Specific Anatomical Regions:
- Upper Limb: Shoulder joint (rotator cuff, glenohumeral joint), elbow joint, wrist and hand (carpal bones, metacarpals, phalanges, common injuries), and nerve pathways.
- Lower Limb: Hip joint, knee joint (menisci, ligaments), ankle and foot (tarsals, metatarsals, phalanges, arches), and nerve pathways.
- Spine: Cervical, thoracic, and lumbar vertebrae, spinal cord and nerve roots, and common spinal conditions like herniated discs, spinal stenosis, and scoliosis.
- Orthopedic Conditions:
- Fractures: Types of fractures, fracture healing, and complications.
- Dislocations: Types of dislocations and joint instability.
- Soft Tissue Injuries: Sprains, strains, tendonitis, and bursitis.
- Arthritis: Osteoarthritis and rheumatoid arthritis.
- Tumors: Bone tumors (e.g., osteosarcoma, chondrosarcoma) and soft tissue tumors.
Medical Biochemistry For Paramedical Course 4 Years
Important topics in Medical Biochemistry include metabolism (carbohydrates, lipids, amino acids, and nucleotides), enzymes, molecular biology (DNA, RNA, gene expression), and the role of vitamins and minerals. Other key areas are bioenergetics, protein structure and function, cell biology, and clinical biochemistry (including liver and kidney function tests).
Here’s a more detailed breakdown:
1. Metabolism:
- Carbohydrate Metabolism:This includes glycolysis, gluconeogenesis, the citric acid cycle, glycogen metabolism, and the pentose phosphate pathway.
- Lipid Metabolism:This covers fatty acid synthesis and breakdown (beta-oxidation), cholesterol metabolism, and the structure and function of lipoproteins.
- Amino Acid Metabolism:This includes amino acid synthesis and degradation, the urea cycle, and the metabolism of specific amino acids like tyrosine and phenylalanine.
- Nucleotide Metabolism:This involves the synthesis and breakdown of purines and pyrimidines.
2. Enzymes:
- Enzyme kinetics (Michaelis-Menten equation, Lineweaver-Burk plot).
- Enzyme regulation (allosteric regulation, covalent modification).
- Examples of enzymes in metabolic pathways.
3. Molecular Biology:
DNA structure and replication, RNA structure and transcription, Protein synthesis (translation), and Gene regulation and the Lac operon.
4. Vitamins and Minerals:
- Water-soluble and fat-soluble vitamins.
- Essential minerals and their roles in the body.
5. Other Important Areas:
- Bioenergetics: The study of energy flow in living organisms.
- Protein Structure and Function: This includes protein folding, domains, and the relationship between structure and function.
- Cell Biology: This includes cell structure, organelles, and membrane transport.
- Clinical Biochemistry: This covers topics like liver and kidney function tests, acid-base balance, and tumor markers.
- Free Radicals and Antioxidants: Oxidative stress and its role in disease.
- Inborn Errors of Metabolism: Lysosomal storage diseases and other metabolic disorders.
6. Specific Topics:
- Glycogen storage diseases.
- Hemoglobin structure and function.
- Hormone action and second messengers.
- Markers enzymes and their significance.
- Clinical disorders related to metabolism (e.g., diabetes).
Essential drugs For Paramedical Course 4 Years
Essential drugs are medications crucial for addressing a population’s priority healthcare needs, selected based on factors like disease prevalence, public health relevance, efficacy, safety, and cost-effectiveness. They must be consistently available within functioning healthcare systems, in appropriate dosage forms, with assured quality, and at affordable prices. Key aspects of essential medicines include selection criteria, procurement and supply, and their role in national health initiatives.
Important Topics Related to Essential Medicines:
- Selection and Prioritization:
- WHO Model List: The World Health Organization (WHO) publishes a model list of essential medicines, which is updated every two years, serving as a guide for countries to develop their own lists.
- National Lists: Countries develop their own essential medicines lists based on their specific disease burden and healthcare needs, often drawing from the WHO model list.
- Criteria for Selection: Essential medicines are chosen based on factors like disease prevalence, public health importance, evidence of efficacy and safety, and cost-effectiveness.
Human Microbiology for Paramedical Course 4 Years
Human microbiology studies the microorganisms (microbes) found in and on the human body, which include bacteria, viruses, fungi, and parasites. This scientific field, often referred to as medical microbiology, focuses on how these microbes interact with humans, whether they are beneficial, harmless, or cause diseases. It involves diagnosing, preventing, and treating infectious diseases caused by these microorganisms, and understanding their pathogenic mechanisms to improve human health.
Key Aspects of Human Microbiology
- Microorganisms Involved:It examines major groups of microbes that can infect or colonize humans, including:
- Bacteria: Such as Helicobacter pylori linked to stomach ulcers.
- Viruses: Including influenza viruses and those causing illnesses like chickenpox.
- Fungi: Like Candida causing conditions such as athlete’s foot and ringworm.
- Parasites: Such as Plasmodium, the parasite that causes malaria.
- Role in Health and Disease:
- Pathogenic Microbes: Some microbes can cause disease, and medical microbiologists are crucial in identifying these agents and developing treatments.
- Beneficial Microbes: The human body also hosts many beneficial microbes, such as those in the gut microbiome, that are vital for health and immune function.
- Diagnostic and Treatment Tools:
- Diagnosis: Microbiologists use techniques like microscopy, culturing, and molecular methods to identify microbes and diagnose infections.
- Treatment: They play a key role in assessing and guiding treatments, often working with other healthcare professionals, to ensure effective therapies.
- Modern Approaches:
- Molecular Microbiology: This subfield focuses on the genotypic (molecular) features of microbes, which has enhanced the diagnosis and management of infectious diseases and provided deeper insights into microbial pathogenesis.
Community Medicine for Paramedical Course 4 Years
Community Medicine is a branch of medicine focused on promoting and protecting the health of entire populations rather than individuals, using strategies like health promotion, disease prevention, and health education to improve community well-being. It applies principles from epidemiology and social and behavioral sciences to address community health needs through strategies such as immunization programs, nutritional campaigns, and environmental health initiatives.
Key Aspects and Goals
- Population Health:Unlike individual patient care, Community Medicine prioritizes the collective health of the community.
- Health Promotion:It involves educating communities on healthy lifestyles, nutrition, physical activity, and preventive measures.
- Disease Prevention and Control:This includes implementing vaccination campaigns, screening programs, and measures to control the spread of both communicable and non-communicable diseases.
- Community Diagnosis and Treatment:Community medicine professionals identify community health problems and develop strategies to address them, often focusing on primary healthcare approaches.
- Application of Diverse Fields:The discipline integrates knowledge from social medicine, public health, epidemiology, environmental health, occupational health, and health policy.
Examples of Interventions
- National Nutritional Campaigns:A community-level approach can more effectively reduce widespread deficiencies like Vitamin A deficiency.
- Public Health Programs:This can involve developing strategies for safe water, sanitation, and vector control to prevent diseases.
- Health Education:Organising health education sessions on topics like immunizations or healthy eating habits.
Role in Medical Education
- Community-Oriented Doctors:The subject aims to produce medical graduates equipped to meet community health needs by providing comprehensive healthcare at the primary level.
- Practical Training:Medical students engage in community-based training, which includes day visits, residential field site training, and study tours to understand real-world health challenges.
ENT Drugs and Pharmacology for Paramedical 4 Years
An otolaryngologist, or ENT doctor, can prescribe a variety of medications to treat conditions of the ears, nose, and throat. These drugs come in different forms, such as oral tablets, nasal sprays, ear drops, and topical creams, depending on the specific condition.

Medications for nose and sinuses
- Antihistamines: Used to relieve symptoms of allergic rhinitis, such as sneezing, itching, and a runny nose.
- Examples: Cetirizine, Loratadine, Desloratadine.
- Intranasal corticosteroids: These nasal sprays reduce inflammation in the nasal passages to treat both allergic and non-allergic rhinitis, as well as nasal polyps.
- Examples: Fluticasone, Mometasone, Budesonide.
- Decongestants: Work by shrinking swollen blood vessels in the nose to relieve congestion from allergies or infections like sinusitis.
- Examples: Oxymetazoline, Pseudoephedrine.
- Antibiotics: Prescribed for bacterial infections such as acute sinusitis.
- Examples: Amoxicillin/clavulanic acid.
Medications for ear conditions
- Antibiotic ear drops: Treat infections of the outer ear, also known as swimmer’s ear (otitis externa).
- Examples: Ciprofloxacin, Ofloxacin.
- Topical steroids for ears: Reduce inflammation and itching in the ear canal caused by allergies or infections.
- Examples: Dexamethasone, Betamethasone.
- Oral antibiotics: For middle ear infections (otitis media) or severe outer ear infections.
- Examples: Amoxicillin, Amoxicillin/clavulanate.
- Wax emulsifiers: Ear drops that soften and loosen earwax buildup to facilitate removal.
- Examples: Carbamide peroxide, Sodium bicarbonate.
- Antifungal ear drops: Prescribed to treat fungal ear infections, such as otomycosis.
- Examples: Clotrimazole.
Medications for throat issues
- Antibiotics: Prescribed for bacterial infections like tonsillitis.
- Examples: Amoxicillin.
- Analgesics/Antipyretics: Over-the-counter pain relievers that treat minor aches, pains, sore throat, and fever.
- Examples: Acetaminophen, NSAIDs (Ibuprofen).
- Antifungal medications: Treat fungal infections in the mouth and throat (oral thrush), often given as a lozenge or gel.
- Examples: Miconazole, Nystatin.
- Cough suppressants (Antitussives) and Expectorants: Treat coughs by suppressing the cough reflex or loosening mucus.
- Examples: Dextromethorphan (suppressant), Guaifenesin (expectorant).
- Anesthetic sprays and lozenges: Provide temporary relief for a sore throat.
- Example: Benzydamine hydrochloride.
Note: Always consult a healthcare professional for a diagnosis and treatment plan. Using these medications without proper guidance may lead to improper treatment or adverse effects.
Ophthalmic Drugs and Pharmacology for Paramedical Course 4 Years
Ophthalmic drugs are medications administered to or around the eye to treat various eye conditions, including infections, glaucoma, inflammation, and dry eye. These medications can include antibacterials, antivirals, antifungals, steroids, glaucoma agents, antihistamines, and tear replacements, and are available in forms such as eye drops, ointments, and hydrogels. Ophthalmic drugs target specific eye structures and aim to reduce intraocular pressure, fight infections, or manage symptoms like pain and redness.
Types of Ophthalmic Drugs
Ophthalmic drugs are categorized based on their function and the conditions they treat:
- Anti-Infectives:Used to treat eye infections caused by bacteria or viruses.
- Examples: Polymyxin B/trimethoprim, erythromycin, and tobramycin are antibacterial agents. Acyclovir is an antiviral medication.
- Anti-Inflammatory Drugs:Used to reduce inflammation, pain, and other symptoms associated with eye inflammation.
- Examples: Steroid eye drops reduce inflammation. Non-steroidal anti-inflammatory drugs (NSAIDs) like ketorolac are also used.
- Glaucoma Therapy:Medications that help to lower intraocular pressure, a common cause of optic nerve damage in glaucoma.
- Examples: Prostaglandin agonists (latanoprost), carbonic anhydrase inhibitors (dorzolamide), and beta-blockers (timolol) are used to treat glaucoma.
- Antihistamines and Decongestants:Used to relieve symptoms of allergies, such as itching, redness, and watery eyes.
- Tear Replacements and Lubricants:Artificial tears or lubricating drops are used to alleviate symptoms of dry eye and improve eye comfort.
- Mydriatics and Cycloplegics:Drugs that dilate the pupil or temporarily paralyze the eye’s ciliary muscle, often used during eye exams.
Delivery Methods
Ophthalmic drugs are typically delivered to the eye through topical forms:
- Eye drops: The most common form of ophthalmic medication.
- Ointments and Gels: Provide a longer-lasting effect and can be used for certain conditions.
- Contact Lenses: Some specialized lenses are designed to release medication over time.
Fungal Infections and Treatment for Paramedical Course 4 Years
Fungal Infections
Fungal infections, or mycoses, are
conditions caused by fungi, a type of living organism distinct from plants or animals. Infections can range from common and mild skin conditions to serious, life-threatening systemic diseases. Fungi are present everywhere in the environment, but infections typically occur when conditions allow fungi to overgrow or enter the body through a weakened immune system or break in the skin.
Types of fungal infections
Fungal infections are generally classified based on the part of the body they affect.
Superficial infections
These are the most common type and affect the outermost layers of the body, such as the skin, hair, and nails.
- Athlete’s foot (tinea pedis): A very common infection of the feet that causes itchy, peeling, and scaly skin, often between the toes.
- Ringworm (tinea corporis): A highly contagious infection of the skin that presents as a red, circular, scaly rash.
- Jock itch (tinea cruris): An itchy rash in the groin, buttocks, and inner thigh area.
- Fungal nail infections (onychomycosis): Causes nails to become thick, discolored, and brittle.
- Candidiasis: Caused by Candida yeast, which normally lives on the body. An overgrowth can cause oral thrush, vaginal yeast infections, and rashes in skin folds.
- Tinea versicolor: Caused by Malassezia yeast, this infection results in discolored skin patches.
Subcutaneous infections
These occur when fungi enter the body through a cut or puncture wound, leading to deep skin and tissue infections.
- Sporotrichosis (“rose gardener’s disease”): Caused by Sporothrix fungus, it can cause skin nodules or ulcers.
- Eumycetoma: A chronic infection that often affects the feet and causes swelling and nodules.
Systemic infections
These are serious, invasive infections that affect internal organs like the lungs, blood, or brain. They are more likely to occur in individuals with a weakened immune system.
- Aspergillosis: Caused by the Aspergillus mold, which can lead to lung infections.
- Invasive candidiasis: A serious infection that can spread to the blood and organs.
- Cryptococcosis: Caused by Cryptococcus fungi, which can affect the lungs and brain, causing meningitis.
- Histoplasmosis: A lung infection caused by inhaling fungal spores, common in certain geographic areas.
Symptoms
Symptoms depend on the type and location of the infection.
- Skin, hair, and nails: Itching, redness, rashes, scaly or cracked skin, and thick or discolored nails.
- Lungs: Coughing (sometimes with blood), fever, fatigue, and shortness of breath.
- Mouth: White patches, pain when eating, or loss of taste (oral thrush).
- Systemic infections: More generalized symptoms like fever, fatigue, muscle aches, and headache.
Risk factors
While anyone can get a fungal infection, certain factors increase the risk.
- Weakened immune system: Conditions like HIV/AIDS, cancer, and immunosuppressant medications reduce the body’s ability to fight off fungi.
- Medical conditions: Diabetes, poor circulation, and other skin conditions like eczema can increase susceptibility.
- Warm, moist environments: Fungi thrive in areas like public showers, locker rooms, and sweaty shoes.
- Antibiotic use: Long-term or high-dose antibiotic use can disrupt the natural balance of microorganisms on the body, allowing fungi to overgrow.
Treatment
Treatment options vary based on the infection’s location and severity.
- Topical medications: For most superficial skin infections, over-the-counter or prescription antifungal creams, lotions, and powders containing ingredients like clotrimazole or terbinafine are used.
- Oral medications: Severe or widespread infections, and those affecting the nails or scalp, may require antifungal pills like fluconazole or terbinafine.
- Antifungal injections: Severe systemic infections may be treated with IV antifungal medications in a hospital setting.
Prevention
Many fungal infections can be prevented through simple hygiene practices.
- Keep skin clean and dry: Thoroughly dry your skin after showering, especially in skin folds and between toes.
- Wear breathable clothing: Opt for loose-fitting, natural fabrics like cotton to prevent moisture buildup.
- Protect your feet: Wear sandals or flip-flops in public showers, gyms, and pool areas.
- Do not share personal items: Avoid sharing towels, clothing, and other personal items with others.
- Manage underlying health: If you have diabetes or other conditions, manage them to help support your immune system.
Medical Diagnosis for Paramedical Course 4 Years
Medical diagnosis is the process of identifying the cause of a person’s health problem, disease, or injury based on their signs and symptoms, patient history, and results from examinations and tests. It is a crucial first step that involves information gathering, analysis, and interpretation to arrive at a definitive conclusion, which then guides appropriate treatment.
The Diagnostic Process
- 1. Patient History:The process begins with the patient reporting their symptoms and medical history.
- 2. Physical Examination:A doctor performs a physical examination, which can include checking vital signs (blood pressure, temperature), listening to the heart and lungs, examining the eyes and mouth, and testing reflexes.
- 3. Tests:To confirm or rule out conditions, various tests may be conducted, such as:
- Laboratory tests: Blood tests, urine tests, and biopsies are common.
- Imaging tests: X-rays, CT scans, and MRIs provide internal views of the body.
- 4. Information Integration and Interpretation:The gathered information from the history, examination, and tests is integrated and interpreted to determine a working diagnosis.
- 5. Differential Diagnosis:In some cases, a doctor may have several potential conditions in mind and uses the process of differential diagnosis to distinguish between them, sometimes by trying treatments for different conditions to see which is most effective.
Purpose of Diagnosis
- Identify the problem: It’s the first step in understanding a health issue.
- Guide treatment: A precise diagnosis is essential for choosing the most effective treatment plan.
- Inform prognosis: A diagnosis helps predict the future course of a disease or condition.
General Surgery for Paramedical Course 4 Years
General surgery is a broad surgical specialty focused on diagnosing and treating a wide range of conditions, primarily involving the abdomen, digestive tract, breast, skin, and endocrine system, such as hernias, gallstones, appendicitis, and thyroid disorders. General surgeons manage the entire surgical process, from diagnosis and pre-operative care to the operation itself and post-operative recovery, often employing minimally invasive techniques.
Key Areas of Focus
- Alimentary Tract & Abdomen:This is a core area, including conditions affecting the esophagus, stomach, small and large intestines, gallbladder, liver, pancreas, and appendix.
- Breast, Skin, & Soft Tissue:General surgeons treat diseases of the breast and various skin and soft tissue disorders, including cancerous growths and other lesions.
- Endocrine System:Procedures involving the thyroid, parathyroid, adrenal glands, and endocrine pancreas fall under their expertise.
- Vascular System:They also manage conditions of the peripheral blood vessels.
- Trauma & Critical Care:General surgeons often play a role in the care of patients with traumatic injuries or other conditions requiring intensive care.
What a General Surgeon Does
- Diagnosis: They use diagnostic tools to identify surgical problems.
- Surgical Treatment: They perform a variety of procedures, ranging from traditional open surgery to minimally invasive laparoscopic techniques.
- Pre- and Post-Operative Care: They manage patient care before, during, and after surgery, including complications.
Common Conditions Treated
- Appendicitis
- Gallstones and other gallbladder diseases/ Cholecystitis
- Hernias
- Conditions of the colon and rectum
- Breast tumors
- Thyroid disorders
- Bowel obstructions
Appendicitis in General Surgery for Paramedical 4 Years
Appendicitis is the inflammation of the appendix, a small pouch attached to the large intestine, usually caused by a blockage. Symptoms include abdominal pain that starts near the belly button and moves to the lower right abdomen, loss of appetite, nausea, and fever. Diagnosis involves medical history, physical exam, and imaging tests, while treatment is almost always surgery to remove the appendix. Complications include ruptured appendix, peritonitis (abdominal lining infection), abscesses, and sepsis. Prevention isn’t generally possible, but prompt treatment of symptoms is crucial to avoid complications.
Definition
- Inflammation of the Appendix:Appendicitis is the inflammation of the appendix, a small, finger-like pouch connected to the large intestine.
- Medical Emergency:It is considered a medical emergency requiring immediate attention because a ruptured appendix can lead to life-threatening infections.
Causes
- Obstruction:The primary cause is an obstruction within the appendix, often from hardened stool (fecalith), undigested food, or other blockages.
- Infection:This blockage can lead to bacterial infection, swelling, and inflammation within the appendix.
Clinical Features (Symptoms)
- Abdominal Pain: The most common symptom, typically starting near the belly button and migrating to the lower right side of the abdomen within hours.
- Nausea and Vomiting: Often follows the onset of pain.
- Loss of Appetite (Anorexia): A common early symptom.
- Low-Grade Fever: May worsen as the condition progresses.
- Increased Pain: Pain that worsens with coughing, walking, or sneezing.
Diagnosis
- Medical History and Physical Exam:A doctor will ask about symptoms and examine the abdomen, checking for signs of tenderness and rigidity.
- Blood Tests:To check for an elevated white blood cell count, which indicates infection.
- Imaging Tests:Ultrasound, CT scan, or MRI can help confirm the diagnosis and rule out other conditions.
Treatment
- Appendectomy (Surgery): The standard treatment is surgery to remove the inflamed appendix, known as an appendectomy.
- Laparoscopic Surgery: Often performed using minimally invasive techniques for a faster recovery.
- Antibiotics: May be used in some cases, particularly for contained abscesses, sometimes followed by surgery.
Complications
- Ruptured Appendix: If the appendix bursts, it spills infectious contents into the abdominal cavity.
- Peritonitis: A serious infection and inflammation of the lining of the abdomen.
- Abscess: A painful pocket of pus that forms around the ruptured appendix.
- Sepsis: A rare but severe complication where bacteria from the abscess enter the bloodstream, potentially leading to a systemic life-threatening infection.
Prevention
- No Direct Prevention:There is no specific way to prevent appendicitis, as it often results from a blockage.
- Prompt Medical Attention:Seeking immediate medical care for symptoms can prevent the appendix from rupturing and developing severe complications.
Cholecystitis in General Surgery for Paramedical Course 4 Years
Cholecystitis is the inflammation of the gallbladder, most often caused by a gallstone obstructing the cystic duct, leading to pain in the upper right abdomen, fever, and nausea. Diagnosis involves imaging tests, with treatment typically including antibiotics, supportive care, and often a cholecystectomy (gallbladder removal). Complications can be severe, including gangrene or perforation of the gallbladder. Prevention focuses on risk factor management, such as maintaining a healthy weight and regular physical activity.
Definition
Cholecystitis is the inflammation of the gallbladder, a small sac that stores bile. It can be acute (sudden) or chronic (long-term) and is usually caused by a gallstone blocking the cystic duct, which impairs bile drainage.
Causes
- Gallstones (Cholelithiasis):The most common cause, where gallstones block the cystic duct, causing bile to build up and lead to inflammation.
- Infection:Bacterial infection can occur when impaired barrier functions allow pathogens to penetrate the gallbladder.
- Other factors:Conditions like serious illnesses (e.g., HIV, diabetes), tumors, or impaired gallbladder emptying can also contribute.
Clinical Features (Symptoms)
- Pain: Sudden, intense pain in the upper right abdomen that may spread to the right shoulder or back.
- Fever: A high temperature is often present.
- Nausea and Vomiting: These are common symptoms associated with cholecystitis.
- Jaundice: Yellowing of the skin and whites of the eyes can occur in some cases.
- Other symptoms: Bloating, sweating, loss of appetite, and tenderness in the upper-right abdomen.
Diagnosis
- Physical Exam: Doctors will check for tenderness in the abdomen.
- Blood Tests: To check for high white blood cell counts and inflammation.
- Imaging:
- Abdominal Ultrasound: To visualize gallstones and gallbladder inflammation.
- CT Scan: Provides more detailed images.
- MRCP: A specific type of MRI to examine the bile ducts.
- Nuclear Imaging (HIDA scan): To assess gallbladder function.
Treatment
- Supportive Care:
- Fasting: To allow the gallbladder to rest.
- Antibiotics: To treat bacterial infections.
- Pain Relief: To manage the intense pain.
- Cholecystectomy (Gallbladder Removal):The definitive treatment for cholecystitis, as it addresses the source of the problem.
Complications
- Gangrene or Tissue Death: Untreated cholecystitis can lead to serious tissue damage.
- Perforation: The gallbladder wall can rupture.
- Abscess: The formation of a pocket of pus.
- Secondary Infections: The inflammation can lead to further bacterial spread.
- Pancreatitis: Inflammation of the pancreas, a potential complication.
Prevention
- Healthy Weight: Maintain a body mass index (BMI) within a healthy range.
- Regular Exercise: Physical activity helps manage weight.
- Diet: Avoid rapid weight loss, which can increase the risk of gallstones.
- Manage Other Conditions: Control diabetes and other risk factors.
Cardiovascular Drugs and Diseases for Paramedical Course 4 Years
Cardiovascular drugs treat a range of heart and blood vessel conditions by acting on the circulatory system to manage blood pressure, heart rate, and cholesterol, and to prevent blood clots. Key drug classes include ACE inhibitors and ARBs for blood pressure and heart failure, beta blockers to slow heart rate and manage angina, diuretics to reduce fluid, statins to lower cholesterol, and anticoagulants to prevent clots.
Categories of Cardiovascular Drugs
- ACE Inhibitors and Angiotensin II Receptor Blockers (ARBs):These drugs treat high blood pressure and heart failure by blocking the effects of angiotensin, a hormone that constricts blood vessels.
- Beta Blockers:These medications slow heart rate, reduce blood pressure, and manage certain arrhythmias by blocking the effects of adrenaline and other stress hormones.
- Diuretics:Also known as “water pills,” these medications remove excess salt and water from the body, which helps to lower blood pressure and reduce fluid buildup in the body.
- Calcium Channel Blockers:These drugs, such as amlodipine, reduce the influx of calcium into heart cells and blood vessels, which helps to lower blood pressure and treat angina (chest pain).
- Anticoagulants (Blood Thinners):These drugs, like warfarin, prevent blood clots from forming in people with chronic cardiac arrhythmias or artificial heart valves.
- Statins:These medications lower high blood cholesterol and other lipids, which reduces the risk of heart disease.
- Vasodilators:These drugs relax and widen blood vessels, improving blood flow and oxygen distribution throughout the body.
Common Uses
Cardiovascular drugs are used to manage or treat:
- High blood pressure (hypertension)
- Heart failure
- High cholesterol (hypercholesterolemia)
- Angina (chest pain)
- Arrhythmias (irregular heartbeats)
- Blood clots
Important Considerations
- A medical expert, such as a doctor, is best equipped to provide personalized information and care.
- Some medications, like certain anticoagulants and beta blockers, require monitoring and should not be stopped suddenly.
- Side effects can occur, and patients with diabetes may need close monitoring, especially when taking beta blockers.
Cardiovascular Disease
Cardiovascular disease (CVD) is
a general term for a group of disorders that affect the heart and blood vessels, including the arteries and veins. CVD is the leading cause of death worldwide.
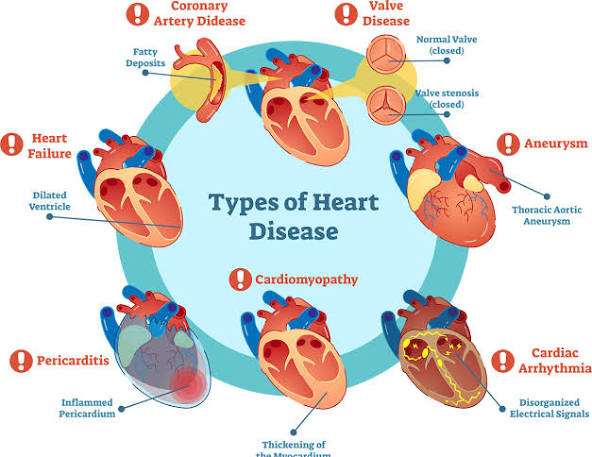

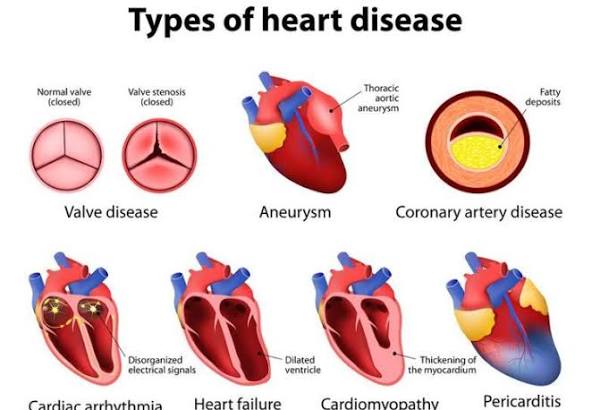

Common types of cardiovascular disease
- Coronary artery disease (CAD): The most common type of CVD, CAD occurs when the arteries supplying the heart muscle become hardened and narrowed due to plaque buildup. This can lead to angina (chest pain), heart attack, and heart failure.
- Cerebrovascular disease: Conditions that affect the blood vessels supplying the brain, including stroke and transient ischemic attacks (TIAs).
- Peripheral artery disease (PAD): This involves blocked or narrowed arteries in the limbs, most often the legs, leading to cramping, pain, and numbness.
- Heart failure: A chronic condition where the heart cannot pump enough blood to meet the body’s needs, leading to fluid buildup and fatigue.
- Arrhythmias: Abnormal heart rhythms that cause the heart to beat too quickly, too slowly, or irregularly.
- Congenital heart disease: Heart defects present at birth.
- Rheumatic heart disease: Damage to the heart muscle and valves from rheumatic fever, a complication of a streptococcal infection.
Symptoms
Symptoms of CVD can vary depending on the specific condition, and some individuals may have no symptoms until a major event, like a heart attack or stroke.
Symptoms of a heart attack:
- Chest pain, pressure, tightness, or discomfort
- Pain or discomfort radiating to the arms (especially the left), jaw, neck, back, or stomach
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or fainting
- Cold sweats
Symptoms of a stroke:
- Sudden numbness or weakness in the face, arm, or leg (usually on one side)
- Confusion or difficulty speaking or understanding speech
- Vision problems in one or both eyes
- Dizziness or loss of balance
- Severe headache with no known cause
Risk factors
Risk factors can be either modifiable (changeable) or non-modifiable (unchangeable).
Modifiable risk factors:
- High blood pressure: Damages blood vessels and strains the heart.
- High cholesterol: Leads to plaque buildup in the arteries (atherosclerosis).
- Tobacco use: Chemicals in tobacco damage the heart and blood vessels.
- Physical inactivity: Increases the risk of obesity, high blood pressure, and high cholesterol.
- Poor diet: Diets high in saturated and trans fats, sugar, and sodium contribute to heart disease.
- Obesity: Especially excess weight around the abdomen, puts extra stress on the heart.
- Diabetes: High blood sugar levels can damage blood vessels over time.
- Excessive alcohol use: Can raise blood pressure and cholesterol levels.
- Unmanaged stress: May increase blood pressure and is linked to unhealthy coping habits.
Non-modifiable risk factors:
- Age: Risk increases with age, particularly after 45 for men and 55 for women.
- Sex: Men are generally at greater risk earlier in life; a woman’s risk increases significantly after menopause.
- Family history: A family history of premature heart disease increases an individual’s risk.
- Ethnicity: Certain ethnic backgrounds have an increased risk.
Prevention and treatment
Prevention focuses on modifying lifestyle risk factors, while treatment varies based on the specific type and severity of the disease.
Prevention strategies:
- Quit smoking and avoid secondhand smoke.
- Eat a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins while limiting saturated fat, sodium, and sugar.
- Engage in regular physical activity, such as 30 minutes of moderate exercise most days of the week.
- Manage underlying health conditions like high blood pressure, high cholesterol, and diabetes.
- Maintain a healthy weight.
- Manage stress through healthy coping mechanisms.
- Get regular health screenings for blood pressure and cholesterol.
Treatment options:
- Lifestyle changes: Similar to prevention, these are often the first line of treatment.
- Medications: A doctor may prescribe drugs like statins, aspirin, or beta-blockers to manage cholesterol, blood pressure, or other symptoms.
- Medical procedures or surgery: Severe cases may require procedures like angioplasty, stenting, or bypass surgery to open blocked arteries or repair heart valves.
- Cardiac rehabilitation: A monitored exercise program to help strengthen the heart after a cardiac event.
Practical Class on Heartbeat
A heartbeat is the rhythmic contraction and relaxation of the heart, driven by electrical signals, pumping blood through the body; it involves phases like diastole (relaxation/filling) and systole (contraction/pumping) and is measured as beats per minute (BPM), with 60-100 BPM being a normal resting range for adults, though it varies with activity. The electrical impulse originates at the sinoatrial (SA) node, travels through the atria, and then to the ventricles, causing them to contract and pump oxygenated and deoxygenated blood.
How it works (The Cardiac Cycle)
- Diastole (Relaxation): The heart’s chambers relax, and blood flows from the body into the right atrium and from the lungs into the left atrium, then into the ventricles.
- Atrial Systole: The atria contract, pushing remaining blood into the ventricles.
- Ventricular Systole: The ventricles contract forcefully, pushing blood out: the right side sends it to the lungs, and the left side pumps it to the rest of the body.
- Cycle Repeats: The heart then re-enters diastole, refilling with blood.
Key Terms
- SA Node: The heart’s natural pacemaker, initiating the electrical signal.
- Pulse: The palpable wave of blood flow from the heart’s beat.
- Heart Rate: The number of beats per minute (BPM).
- Tachycardia: A heart rate over 100 BPM at rest.
- Bradycardia: A slow heart rate (not mentioned in snippets, but implied opposite of tachycardia).
What affects it
- Factors Such as Stress, caffeine, nicotine, exercise, and hormones can increase heart rate.
- Normal Range: 60-100 BPM at rest for most adults, though athletes often have lower rates.
Practical Class on Heart Rate
Heart rate is the number of times your heart beats per minute (bpm), with a normal resting rate for adults generally being 60-100 bpm, though it varies with age, fitness, stress, and medications, with athletes often having lower rates. It’s a key health indicator, reflecting heart function; a consistently high rate (tachycardia, >100 bpm at rest) or low rate (bradycardia, <60 bpm at rest, unless fit) can signal issues. You can check it by feeling your pulse at the wrist or with devices, ideally after resting.
Normal Ranges & Factors
- Adults: 60-100 bpm resting.
- Athletes: Can be as low as 40 bpm or less.
- Children: Have higher rates, e.g., 80-120 bpm for ages 3-5.
- Factors Affecting It: Fitness, emotions, caffeine, alcohol, medications, illness, pregnancy, and sleep quality.
How to Check Your Heart Rate
- Rest: Sit quietly for 5-10 minutes.
- Locate Pulse: Place index and middle fingers on the thumb side of your wrist.
- Count: Count beats for 15 seconds and multiply by 4, or count for a full minute.
- Devices: Smartwatches and fitness trackers offer easy monitoring.
Practical Class on Tachycardia
Tachycardia is a heart rhythm disorder where the heart beats too fast, typically over 100 beats per minute (bpm) at rest in adults, signaling an electrical problem or normal response to stress, exercise, or underlying conditions like fever, anemia, anxiety, or thyroid issues, causing symptoms like palpitations, dizziness, and shortness of breath, requiring medical evaluation to determine if it’s benign (sinus tachycardia) or a serious arrhythmia needing treatment.
Types of Tachycardia
- Sinus Tachycardia: A normal response to stress, fever, or exercise, where the sinus node fires too quickly.
- Supraventricular Tachycardia (SVT): Abnormal signals start above the ventricles, causing sudden, rapid heartbeats, often felt as palpitations.
- Ventricular Tachycardia (VT): A dangerous rhythm originating in the heart’s lower chambers, potentially life-threatening.
- Atrial Fibrillation (AFib) & Flutter: Irregular, rapid heartbeats in the upper chambers (atria).
Common Symptoms
Racing heart or palpitations, Dizziness or lightheadedness, Shortness of breath, and Chest pain or discomfort.
Common Causes & Triggers
- Lifestyle: Caffeine, alcohol, stimulants, smoking, stress, lack of sleep.
- Medical Conditions: Fever, anemia, thyroid disease, dehydration, lung disease, sleep apnea, heart disease, and high blood pressure.
- Electrical Issues: Faulty heart wiring or triggers in the heart’s chambers.
Practical Class on Bradycardia
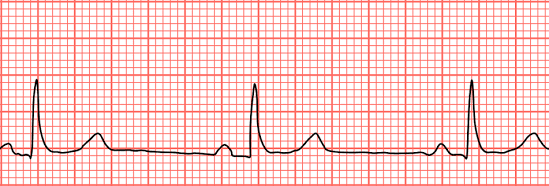

Bradycardia is a slower-than-normal heart rate, typically under 60 beats per minute (bpm) in adults at rest, caused by issues with the heart’s electrical system, certain medications, or underlying conditions like sleep apnea or thyroid problems, leading to symptoms like dizziness, fatigue, shortness of breath, and confusion, though highly fit individuals and athletes may have a normal slow rate. Treatment varies by cause, ranging from lifestyle changes to pacemakers, and involves diagnosing the underlying problem with tools like an EKG.
What it is
- A heart rate below 60 bpm, meaning the heart isn’t pumping enough oxygen-rich blood to the body.
- Can be normal for athletes or during sleep, but problematic if it causes symptoms.
Common types
- Sinus Bradycardia: Slowing of the heart’s natural pacemaker (sinus node).
- Heart Block: Electrical signals from the upper to lower heart chambers are blocked.
Causes
- Heart Issues: Heart disease, previous heart attacks, sick sinus syndrome.
- Medications: Beta-blockers, calcium channel blockers.
- Medical Conditions: Thyroid problems, electrolyte imbalances, sleep apnea, and inflammation.
- Lifestyle: Intense physical fitness (often normal), aging.
Symptoms (when problematic)
- Dizziness, lightheadedness, fainting.
- Fatigue, weakness.
- Shortness of breath, chest pain.
- Confusion or memory problems.
Diagnosis & Treatment
- Diagnosis: Physical exam, EKG, Holter monitor, sleep study, blood tests.
- Treatment: Addressing the cause (e.g., changing meds, treating sleep apnea) or using a pacemaker for severe cases.
Practical Class on IM Injection Pushing
The process of pushing an intramuscular (IM) injection involves a smooth, steady depression of the plunger after the needle is securely in the muscle, ensuring the medication goes in slowly to minimize discomfort, followed by quickly withdrawing the needle at the same angle and activating the safety device, then applying gentle pressure to the site with gauze. Key steps include site preparation (cleaning, Z-track method), swift 90-degree needle insertion, slow plunger push (counting to three), quick withdrawal, and immediate disposal in a sharps container.
Pre-Injection Steps (Preparation)
- Hand Hygiene & Supplies: Wash hands thoroughly and gather medication, syringe, alcohol swabs, gauze, and a sharps container.
- Site Selection & Prep: Locate the correct muscle (e.g., deltoid, ventrogluteal), clean with an alcohol swab, and let it dry.
- Z-Track Method (Optional but Recommended): Use your non-dominant hand to pull the skin and tissue to the side to prevent medication leakage into subcutaneous tissue.
- Syringe Prep: Remove the cap, ensure no large air bubbles, and tap to get a drop of medication at the tip.
The “Push” (Injection)
- Insertion: Hold the syringe like a dart and insert the needle quickly at a 90-degree angle into the muscle.
- Stabilize: Once in the muscle, use your non-dominant hand to steady the syringe.
- Depress Plunger: Slowly and steadily push the plunger all the way down, counting to three.
- Withdrawal: After the fluid is in, hold for a few seconds (around 10 for some meds), then pull the needle straight out at the same 90-degree angle.
Post-Injection Steps
- Safety: Immediately activate the needle’s safety shield and dispose of the entire syringe in the sharps container.
- Site Care: Apply gentle pressure with gauze or a cotton ball (no rubbing) and secure with a bandage if needed.
- Observe: Monitor the patient for any adverse reactions.
Process of IV Injection Pushing
The process of IV Injection Pushing (or Bolus) involves a trained healthcare professional manually injecting medication directly into an established IV line using a syringe, following strict steps: verify order, prepare patient, scrub the IV port (clave), flush with saline to check for patency, attach the medication syringe, push the drug at a specific rate (seconds to minutes) while monitoring, and then perform a post-flush to clear the line, ensuring patient safety and proper delivery.
Key Steps in IV Push Administration
- Preparation & Verification:
- Confirm the doctor’s order, patient details, medication rights (right drug, dose, time, route, patient, documentation, reason, response).
- Gather supplies: saline flush, medication syringe, alcohol wipes, and gloves.
- Perform hand hygiene and don gloves.
- Educate the patient about the medication and potential side effects.
- Priming & Flushing (SASH Method):
- Saline Flush: Scrub the injection port (clave) with an alcohol wipe for 15-30 seconds, let it air dry, then inject 3-5mL of saline to check for patency (blood return) and clear the line.
- Medication Administration:
- Attach Medication: Attach the pre-filled medication syringe (air expelled) to the scrubbed port and twist clockwise to secure.
- Slow Push: Slowly inject the medication at the prescribed rate (e.g., over 1 minute, 2 minutes). Use a timer for accuracy; break down the volume into smaller intervals for easier pacing (e.g., 0.5mL every 30 seconds for a 1mL/min push).
- Completion (SASH):
- Follow-up Flush: After the medication, flush with another 3-5mL of saline at the same rate as the medication push to ensure all the drug enters the bloodstream and clears the tubing, preventing incompatibility with other IV fluids.
- Secure the port with a new alcohol cap if required by facility policy.
Important Considerations
- Timing is Crucial: Pushing too fast can cause adverse effects or medication waste; too slow might delay treatment.
- Compatibility: Always check if the medication is compatible with the primary IV fluid running, if any.
- Patient Monitoring: Closely watch the patient for any adverse reactions during and after administration, especially respiratory changes, notes LevelUpRN.
 HRTD Medical Institute
HRTD Medical Institute





